The influence of extreme cold ambient temperature on out of hospital cardiac arrest: A systemic review and meta-analysis
doi: 10.2478/fzm-2022-0025
-
Abstract:
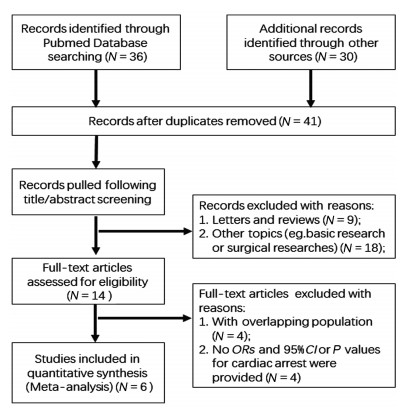
Objective Many researches have demonstrated the effects of the extreme cold ambient temperature on the risk of out-of-hospital cardiac arrest (OHCA); yet, the results have been inconsistent. We performed a meta-analysis to evaluate whether extreme cold ambient temperature is related to OHCA. Methods We searched for time-series studies reporting associations between extreme cold ambient temperature and OHCA in PubMed, web of science and Cochrane database. Results Six studies involving 2 337 403 cases of OHCA were qualified for our meta-analysis. The odds ratio (OR) of OHCA was significantly increased in extreme cold weather (defined as the 1st or 5th centile temperature year-round) compared to reference temperature (as the 25th centile temperatures or daily mean temperature with minimum risk of OHCA) (OR=1.49, 95% CI 1.18-1.88). The subgroup analysis for the elderly and the female failed to detect the influence of extreme cold weather on OHCA, the ORs are 1.25 (95% CI 0.89-1.75) and 1.19 (95% CI 0.87-1.64), respectively. Conclusion The risk of OHCA is significantly higher in extreme cold ambient temperatures than in reference temperature, according to a relative temperature scale with percentiles of the regionspecific temperature distribution. -
Key words:
- extreme cold weather /
- cardiac arrest /
- meta-analysis
-
Table 1. Characteristics of enrolled studies
Study cohort Study range Study region Study type Sample Definition of extreme cold & Temperature Reference Outcome OR or RR (95% CI) Borghei, et al. 2020[6] 3 years
(unspecified)Rasht in Iran single center time-series study 392 the 5th centile temperature, 5℃ the 25th centile temperatures OHCA 1.31 (1.01-1.52) Chen, et al. 2014[7] 2009-2011 6 cities in China multi-center time-series study 126 925 the 1st centile temperatures, -24.2℃-7.9℃ the 25th centile temperatures OHCA 1.33 (1.20-1.47) Medina-Ramon, et al. 2006[8] 1989-2000 50 cities in US multi-center time-series study 1 542 351 the 1st centile temperatures -17.2℃-10℃ the 25th centile temperatures OHCA 1.14 (1.05-1.23) Niu, et al. 2016[9] 2008-2012 Guangzhou, China multi-center time-series study 4 369 the 1st centile temperatures, 6.8℃ 28℃ [daily mean temperature with minimum risk] OHCA 2.85 (1.44-5.63) Onozuka, et al. 2017[10] 2005-2014 47 prefectures in Japan multi-center time-series study 659 752 the 1st centile temperatures, - the 84th centile temperatures [minimum risk] OHCA 2.10 (1.84-2.40) Ryti, et al. 2017[11] 1961-2011 Oulu in Finland multi-center time-series study 3 614 the 5th centile temperature, -9.2℃ reference periods of the same calendar days of other years Sudden cardiac death 1.33 (1.00-1.78) OHCA, out-of-hospital cardiac arrest. Table 2. Assessment of methodological quality of included studies
Item Medina-Ramón, et al. 2006 [8] Chen, et al.2014 [7] Niu, et al.2016 [9] Onozuka, et al. 2017 [10] Ryti, et al.2017 [11] Borghei, et al.2020 [6] 1 Define the source of information (survey, record review) Yes Yes Yes Yes Yes Yes 2 List inclusion and exclusion criteria for exposed and unexposed subjects (cases and controls) or refer to previous publications Yes Yes Yes Yes Unclear Yes 3 Indicate time period used for identifying patients Yes Yes Yes Yes Yes Yes 4 Indicate whether or not subjects were consecutive if not population-based Yes Yes Yes Yes Yes Yes 5 Indicate if evaluators of subjective components of study were masked to other aspects of the status of the participants Yes Yes Yes Yes Yes Yes 6 Describe any assessments undertaken for quality assurance purposes (e.g., test/retest of primary outcome measurements) Yes No Yes Yes Yes No 7 Explain any patient exclusions from analysis Yes Yes No No Yes Yes 8 Describe how confounding was assessed and/or controlled Yes Yes Yes Yes No Yes 9 If applicable, explain how missing data were handled in the analysis No Yes No No No No 10 Summarize patient response rates and completeness of data collection Yes Yes Yes Yes Yes Yes 11 Clarify what follow-up, if any, was expected and the percentage of patients for which incomplete data or follow-up was obtained Yes Yes Yes Yes Yes Yes Total score 10 10 9 9 8 9 Score 0-3 represents for literature with low quality, 4-7 for moderate quality and 8-11 for high quality. -
[1] Yan S, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care, 2020; 24(1): 61. doi: 10.1186/s13054-020-2773-2 [2] Zhang S. Sudden cardiac death in China: current status and future perspectives. Europace, 2015; 17(Suppl 2): ii14-ii18. doi: 10.1093/europace/euv143 [3] Sun Z, Chen C, Xu D, et al. Effects of ambient temperature on myocardial infarction: A systematic review and meta-analysis. Environ Pollut, 2018; 241(1): 1106-1114. [4] Pouwels S, Van Genderen M E, Kreeftenberg H G, et al. Utility of the cold pressor test to predict future cardiovascular events. Expert Rev Cardiovasc Ther, 2019; 17(4): 305-318. doi: 10.1080/14779072.2019.1598262 [5] Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med, 2009; 6(7): e1000097. doi: 10.1371/journal.pmed.1000097 [6] Borghei Y, Moghadamnia M T, Sigaroudi A E, et al. Association between climate variables (cold and hot weathers, humidity, atmospheric pressures) with out-of-hospital cardiac arrests in Rasht, Iran. J Therm Biol, 2020; 93(1): 102702. [7] Chen R, Li T, Cai J, et al. Extreme temperatures and out-ofhospital coronary deaths in six large Chinese cities. J Epidemiol Community Health, 2014; 68(12): 1119-1124. doi: 10.1136/jech-2014-204012 [8] Medina-Ramón M, Zanobetti A, Cavanagh D P, et al. Extreme temperatures and mortality: assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ Health Perspect, 2006; 114(9): 1331-1336. doi: 10.1289/ehp.9074 [9] Niu Y, Chen R, Liu C, et al. The association between ambient temperature and out-of-hospital cardiac arrest in Guangzhou, China. Sci Total Environ, 2016; 572(1): 114-118. [10] Onozuka D, Hagihara A. Extreme temperature and out-of-hospital cardiac arrest in Japan: A nationwide, retrospective, observational study. Sci Total Environ, 2017; 575(1): 258-264. [11] Ryti N R I, Mäkikyrö E M S, Antikainen H, et al. Risk of sudden cardiac death in relation to season-specific cold spells: a casecrossover study in Finland. BMJ Open, 2017; 7(11): e017398. doi: 10.1136/bmjopen-2017-017398 [12] Nakanishi N, Nishizawa S, Kitamura Y, et al. Circadian, weekly, and seasonal mortality variations in out-of-hospital cardiac arrest in Japan: analysis from AMI-Kyoto Multicenter Risk Study database. Am J Emerg Med, 2011; 29(9): 1037-1043. doi: 10.1016/j.ajem.2010.06.018 [13] Curriero F C, Heiner K S, Samet J M, et al. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol, 2002; 155(1): 80-87. doi: 10.1093/aje/155.1.80 [14] O'Neill M S, Zanobetti A, Schwartz J. Modifiers of the temperature and mortality association in seven US cities. Am J Epidemiol, 2003; 157(12): 1074-1082. doi: 10.1093/aje/kwg096 [15] Hua W, Zhang L F, Wu Y F, et al. Incidence of sudden cardiac death in China: analysis of 4 regional populations. J Am Coll Cardiol, 2009; 54(12): 1110-1118. doi: 10.1016/j.jacc.2009.06.016 [16] Cagle A, Hubbard R. Cold-related cardiac mortality in King County, Washington, USA 1980-2001. Ann Hum Biol, 2005; 32(4): 525-537. doi: 10.1080/03014460500153758 [17] Ghaffari S, Pourafkari L. Coronary spasm provocation with cold pressor test. Intern Emerg Med, 2010; 5(6): 559-560. doi: 10.1007/s11739-010-0386-5 [18] Di Blasi C, Renzi M, Michelozzi P, et al. Association between air temperature, air pollution and hospital admissions for pulmonary embolism and venous thrombosis in Italy. Eur J Intern Med, 2022; 96(1): 74-80. [19] Li Y, Ji C, Ju H, et al. Impact of ambient temperature and atmospheric evaporation on the incidence of acute deep venous thrombosis in the northeast of China. Int Angiol, 2017; 36(3): 243-253. [20] Stewart S, Moholdt T T, Burrell L M, et al. Winter peaks in heart failure: an inevitable or preventable consequence of seasonal vulnerability? Card Fail Rev, 2019; 5(2): 83-85. [21] Houdas Y, Deklunder G, Lecroart J L. Cold exposure and ischemic heart disease. Int J Sports Med, 1992; 13 (Suppl 1): S179-S181. -


 投稿系统
投稿系统


 下载:
下载: