Study on the status and countermeasures of disease self-management ability in chronic kidney disease patients in cold regions
doi: 10.1515/fzm-2025-0002
-
Abstract:
Objective Effective Chronic Kidney Disease (CKD) management is particularly important in cold regions of China, where climate and lifestyle factors play significant roles. However, there is a lack of relevant studies in this area. Therefore, the purpose of this study was: (1) to assess the status of self-management capacity in individuals with CKD in cold regions of China and analyze the factors influencing it; (2) to identify strategies to improve CKD management in primary care settings in these regions; and (3) to understand patients' attitudes toward eHealth services. Methods This was a regional, cross-sectional observational study. A questionnaire measuring CKD patients' self-management abilities was derived from the Perceived Kidney Disease Self-Management Scale, the Kidney Disease Behavioral Inventory (KDBI), and the Health Literacy Questionnaire. Data were collected from hospitalized CKD patients in Heilongjiang Province and analyzed using One-Way Analysis of Variance (ANOVA), Hierarchical Regression Analysis, and K-prototype cluster analysis. Results A total of 957 participants were tested. Of these, 70.64% had less than a bachelor's degree, and 56.27% had been diagnosed with hypertensive or diabetic nephropathy. The KDBI scale showed a lower overall score compared to the PKDSMS. Factors such as CKD stage 4 (F = 2.367, P = 0.042), last year's medical expenses (F = 3.974, P = 0.004), and poor self-rated health (F = 33.352, P < 0.01) were found to influence scores on both scales. The health literacy questionnaire revealed significant differences (P < 0.01) in health knowledge, except by sex. Additionally, healthcare expenditures and poor self-rated health were negatively associated with self-management capacity. Conclusions This study provides valuable insights into the self-management challenges faced by CKD patients in cold regions of China. Despite some difficulties in improving self-management, patients showed positive attitudes toward enhancing CKD management services in primary care and developing digital management tools. These findings offer useful references and recommendations for future clinical practice and research in this field. -
Table 1. Demographic characteristics and clinical characteristics of the study samples
Characteristic Number (N) Percent (%) Characteristic Number (N) Percent (%) Sex CKD Cost, RMB Male 527 55.07 ≤ 5000 131 13.69 Female 430 44.93 5000-9000 151 15.78 Education background 10, 000-29, 999 298 31.14 Junior high school or below 378 39.50 30, 000-49, 999 139 14.52 High school or vocational school 298 31.14 ≥ 50, 000 238 24.87 Bachelor's degree or associate degree 268 28.00 Basic health insurance type Master's degree or above 13 1.36 Urban employee basic medical insurance 584 61.02 CKD stage Urban and rural resident basic medical insurance 205 21.42 1 (eGFR > 90mL/[min·1.73m2]) 72 7.52 New rural cooperative medical insurance 128 13.38 2 (eGFR 60-89mL/[min·1.73m2]) 51 5.33 Other 40 4.18 3 (eGFR = 30–60 mL/[min·1.73m2]) 59 6.17 Self-Rated Health 4 (eGFR < 30 mL/[min·1.73m2]) 38 3.97 Very good 208 21.73 5 (eGFR < 15mL/[min·1.73m2])/(Uremic stage) 631 65.94 Good 286 29.89 Uncertain 106 11.08 Fair 305 31.87 CKD duration, years Poor 130 13.58 < 1 144 15.05 Very poor 28 2.93 1-3 (Including 1) 242 25.29 CKD type 3-5 (Including 3) 175 18.29 Diabetic Nephropathy 238 24.87 5-10 (Including 5) 193 20.17 Hypertensive Nephropathy 266 27.80 ≥ 10 203 21.21 Glomerulonephritis 187 19.54 Kidney replacement therapy duration (dialysis or transplant), years Tubulointerstitial Disease 20 2.09 No replacement treatment 272 28.42 Hereditary kidney Disease 48 5.02 < 1 151 15.78 Renal Vascular Disease 4 0.42 1-3 (Including 1) 238 24.87 Autoimmune Disease-related Kidney Disease 20 2.09 3-5 (Including 3) 104 10.87 Infectious Kidney Disease 9 0.94 5-10 (Including 5) 136 14.21 Tumor-related Kidney Disease 12 1.25 ≥ 10 56 5.85 Other 153 15.99 Table 2. Scores for each questionnaire on self-management in CKD patients
PKDSMS Item M SD *It is difficult for me to find effective solutions for problems that occur with my kidney disease (dialysis). 2.550 1.436 *I find efforts to change things I donn't like about my kidney disease (dialysis) are ineffective. 2.652 1.442 I handle myself well with respect to my kidney disease (dialysis). 3.955 1.101 I am able to manage things related to my kidney disease (dialysis) as well as most other people. 4.086 1.051 I succeed in the projects I undertake to manage my kidney disease (dialysis). 4.097 1.029 *Typically, my plans for managing my kidney disease (dialysis) don't work out well. 2.683 1.349 *No matter how hard I try, managing my kidney disease (dialysis) doesn't turn out the way I would like. 2.735 1.403 I am generally able to accomplish my goals with respect to managing my kidney disease (dialysis). 3.811 1.147 * = Item reverse-scored. Cronbach's α = 0.062, KMO = 0.819. Table 3. The health literacy questionnaire score
Health literacy questionnaire Item (Multiple Choice Question) Response Prevalence Rate (%) Number (N) Response Rate (%) 1. When reading written materials such as health manuals and drug instructions related to chronic kidney disease provided by hospitals or pharmacies, have you encountered the following situations? I found the text too small and it was very difficult to read. 489 35.10 51.10 I felt that there were too many professional terms and the content was complicated and difficult to 524 37.62 54.75 understand. I needed someone to help me read or interpret the content. 380 27.28 39.71 I was able to extract the content I needed from the information I collected. 501 20.59 52.35 I understood the CKD information I obtained. 221 9.08 23.09 I have conveyed my views and understanding of chronic kidney disease to others (doctors, patients, relatives and friends). 448 18.41 46.81 I applied the information about chronic kidney disease (life, diet, etc.) I obtained to my daily life. 603 24.78 63.01 Table 4. The status of self-management behaviors among CKD patients
KDBI Item M SD Checked your blood pressure at home 4.051 0.973 Checked your weight changes 4.175 0.943 Monitored weather changes 4.069 1.002 Kept track of laboratory results related to your kidney disease 4.186 0.957 Kept track of symptoms related to your kidney disease 4.083 1.015 Kept track of thoughts and feelings about your health 3.524 1.205 Taken medications as prescribed 4.575 0.719 *Taken a medication in different ways than prescribed 3.664 1.337 *Not taken a prescribed medication 3.841 0.976 Taken herbs, non-prescribed vitamins, or other natural remedies 1.964 1.169 Followed your kidney diet plan 3.962 0.970 Chosen healthier food to eat 4.109 0.974 Exercised for more than 60 minutes each week 3.259 1.294 Taken time to unwind and feel better 3.340 1.213 *Missed dialysis treatments 4.613 0.741 *Missed visits with your doctor 4.391 0.911 * = Item reverse-scored, Cronbach's α = 0.786, KMO = 0.839. Table 5. Analysis of variation between participant characteristics and PKDSMS
Item M±SD t/F P Sex -1.443 0.149 Male (N = 527) 3.29 ± 0.68 Female (N = 430) 3.36 ± 0.69 Education background 2.001 0.112 Junior high school or below (N = 378) 3.27 ± 0.66 High school or vocational school (N = 298) 3.30 ± 0.68 Bachelor's degree or associate degree (N = 268) 3.40 ± 0.72 Master's degree or above (N = 13) 3.41 ± 0.57 CKD stage 2.367 0.042 1 (eGFR > 90mL/[min·1.73m2]) (N = 72) 3.38 ± 0.76 2(eGFR = 60-89mL/[min·1.73m2]) (N = 51) 3.46 ± 0.78 3(eGFR = 30-60 mL/[min·1.73m2]) (N = 59) 3.25 ± 0.63 4 (eGFR < 30 mL/[min·1.73m2]) (N = 38) 3.05 ± 0.55 5 (eGFR < 15mL/[min·1.73m2])/(Uremic stage) (N = 631) 3.33 ± 0.69 Uncertain (v106) 3.33 ± 0.62 CKD duration, years 2.179 0.069 < 1(N=144) 3.35 ± 0.59 1-3 (Including 1) (N = 242) 3.28 ± 0.71 3-5 (Including 3) (N = 175) 3.26 ± 0.70 5-10 (Including 5) (N = 193) 3.29 ± 0.70 ≥ 10 (N = 203) 3.44 ± 0.68 Kidney replacement therapy duration (dialysis or transplant), years 0.899 0.481 No replacement treatment (N = 272) 3.30 ± 0.67 < 1(N=151) 3.30 ± 0.67 1-3 (Including 1) (N = 238) 3.31 ± 0.69 3-5 (Including 3) (N = 104) 3.31 ± 0.69 5-10 (Including 5) (N = 136) 3.33 ± 0.72 ≥10(N=56) 3.50 ± 0.67 CKD Cost, RMB 3.974 0.004 ≤ 5000 (N = 131) 3.48 ± 0.69 500-9000 (N = 151) 3.43 ± 0.73 10, 000-29, 999 (N = 298) 3.24 ± 0.64 30, 000-49, 999 (N = 139) 3.29 ± 0.71 ≥ 50, 000 (N = 238) 3.28 ± 0.68 Basic health insurance type 2.328 0.077 Urban employee basic medical insurance (N = 584) 3.35 ± 0.71 Urban and rural resident basic medical insurance (N = 205) 3.33 ± 0.66 New rural cooperative medical insurance (N = 128) 3.20 ± 0.63 Other (N = 40) 3.22 ± 0.58 Self-Rated Health 33.352 < 0.010 Very good (N = 208) 3.59 ± 0.75 Good (N = 286) 3.49 ± 0.65 Fair (N = 305) 3.18 ± 0.58 Poor (N = 130) 2.93 ± 0.55 Very poor (N = 28) 2.92 ± 0.74 CKD type 10.141 < 0.010 Diabetic Nephropathy (N = 238) 3.21 ± 0.66 Hypertensive Nephropathy (N = 266) 3.33 ± 0.6 Glomerulonephritis (N = 187) 3.33 ± 0.73 Tubulointerstitial Disease (N = 20) 3.26 ± 0.64 Hereditary kidney Disease (N = 48) 3.46 ± 0.63 Renal Vascular Disease (N = 4) 2.97 ± 0.06 Autoimmune Disease-related Kidney Disease (N = 20) 3.29 ± 0.90 Infectious Kidney Disease (N = 9) 3.24 ± 0.55 Tumor-related Kidney Disease (N = 12) 3.29 ± 0.37 Other (N = 153) 3.45 ± 0.73 *P < 0.05, **P < 0.01. Table 6. Analysis of variation between participant characteristics and KDBI
Item M±SD t/F P Sex -0.690 0.491 Male (N = 527) 3.85 ± 0.49 Female (N = 430) 3.88 ± 0.53 Education background 0.075 0.974 Junior high school or below (N = 378) 3.86 ± 0.51 High school or vocational school (N = 298) 3.86 ± 0.53 Bachelor's degree or associate degree (N = 268) 3.87 ± 0.49 Master's degree or above (N = 13) 3.82 ± 0.29 CKD stage 2.622 0.023* 1 (eGFR > 90mL/[min·1.73m2]) (N = 72) 3.86 ± 0.48 2 (eGFR = 60-89mL/[min·1.73m2]) (N = 51) 3.93 ± 0.44 3 (eGFR = 30–60 mL/[min·1.73m2]) (N = 59) 3.96 ± 0.45 4 (eGFR < 30 mL/[min·1.73m2]) (N = 38) 3.79 ± 0.44 5 (eGFR < 15mL/[min·1.73m2])/(Uremic stage) (N = 631) 3.88 ± 0.50 Uncertain (N = 106) 3.72 ± 0.60 CKD duration, years 0.880 0.475 < 1(N=144) 3.82 ± 0.55 1-3 (Including 1) (N = 242) 3.88 ± 0.50 3-5 (Including 3) (N = 175) 3.88 ± 0.52 5-10 (Including 5) (N = 193) 3.90 ± 0.48 ≥ 10 (N = 203) 3.82 ± 0.49 Kidney replacement therapy duration (dialysis or transplant), years 1.554 0.170 No replacement treatment (N = 272) 3.83 ± 0.53 < 1(N=151) 3.81 ± 0.48 1-3 (Including 1) (N = 238) 3.93 ± 0.50 3-5 (Including 3) (N = 104) 3.88 ± 0.46 5-10 (Including 5) (N = 136) 3.89 ± 0.49 ≥10(N=56) 3.80 ± 0.59 CKD Cost, RMB 0.204 0.936 ≤ 5000 (N = 131) 3.84 ± 0.59 5000-9000 (N = 151) 3.87 ± 0.51 10, 000-29, 999 (N = 298) 3.85 ± 0.51 30, 000-49, 999 (N = 139) 3.88 ± 0.47 ≥ 50, 000 (N = 238) 3.88 ± 0.48 Basic health insurance type 2.565 0.053 Urban employee basic medical insurance (N = 584) 3.89 ± 0.49 Urban and rural resident basic medical insurance (N = 205) 3.85 ± 0.46 New rural cooperative medical insurance (N = 128) 3.83 ± 0.56 Other (N = 40) 3.67 ± 0.67 Self-Rated Health 8.203 0** Very good (N = 208) 3.98 ± 0.52 Good (N = 286) 3.93 ± 0.49 Fair (N = 305) 3.79 ± 0.50 Poor (N = 130) 3.73 ± 0.47 Very poor (N = 28) 3.80 ± 0.55 CKD type 0.837 0.582 Diabetic Nephropathy (N = 238) 3.85 ± 0.50 Hypertensive Nephropathy (N = 266) 3.88 ± 0.51 Glomerulonephritis (N = 187) 3.85 ± 0.48 Tubulointerstitial Disease (N = 20) 3.85 ± 0.49 Hereditary kidney Disease (N = 48) 3.96 ± 0.35 Renal Vascular Disease (N = 4) 3.63 ± 0.34 Autoimmune Disease-related Kidney Disease (N = 20) 3.82 ± 0.64 Infectious Kidney Disease (N = 9) 3.88 ± 0.32 Tumor-related Kidney Disease (N = 12) 4.10 ± 0.48 Other (N = 153) 3.82 ± 0.57 *P < 0.05, **P < 0.01. Table 7. Stratified regression analysis of factors influencing self-management on PKDSMS
Characteristics Layer 1 Layer 2 Layer 3 Layer 4 P P P P Sex 0.006 Education Background CKD Cost, RMB Basic health insurance type CKD duration, years Kidney replacement therapy duration(dialysis or transplant), years Self-Rated Health CKD stage CKD type △R2 0.019 0.012 0.114 0.013 Different colours represent the layering of different items. For details, refer to Appendix 3. Table 8. Stratified regression analysis of factors influencing self-management on KDBI
Characteristics Layer 1 Layer 2 Layer 3 Layer 4 P P P P Sex Education Background CKD Cost, RMB Basic health insurance type CKD duration, years Kidney replacement therapy duration (dialysis or transplant), years Self-Rated Health P < 0.01 CKD stage CKD type △R2 0.007 0.009 0.042 0.021 Different colours represent the layering of different items. For details, refer to Appendix 3. Table 9. PKDSMS and KDBI Mean Scores in different clusters of patients
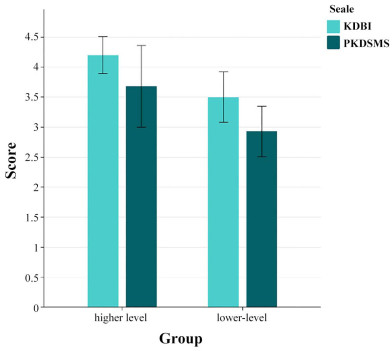
Clusters of patients KDBI PKDSMS Higher level (N = 498) 4.20 ± 0.31 3.68 ± 0.68 Lower level (N = 459) 3.50 ± 0.42 2.93 ± 0.42 F 875.812 411.771 P P < 0.01 P < 0.01 Table 10. Cross-covariance analysis for different clusters
Item Higher Level Lower Level Total χ2 P Willingness to receive CKD diagnosis and treatment at primary health care institutions 25.378 < 0.01 Very willing 181 (36.35) 113 (24.62) 294 (30.72) Willing 95 (19.08) 133 (28.98) 228 (23.82) Uncertain 88 (17.67) 105 (22.88) 193 (20.17) Unwilling 83 (16.67) 72 (15.69) 155 (16.20) Very unwilling 51 (10.24) 36 (7.84) 87 (9.09) Willingness to download and install a mobile health management application 36.942 < 0.01 Very willing 273 (54.82) 164 (35.73) 437 (45.66) Willing 131 (26.31) 167 (36.38) 298 (31.14) Uncertain 58 (11.65) 89 (19.39) 147 (15.36) Unwilling 16 (3.21) 15 (3.27) 31 (3.24) Very unwilling 20 (4.02) 24 (5.23) 44 (4.60) Table 11. Attitude of using smart device among CKD patients in frigid zone
Item Response Prevalence Rate (%) Number (N) Response Rate (%) If you are willing to use the app, which features would you prioritize? (Multiple Choice question) Disease monitoring and alerting 702 25.25 73.35% Health consultation and lifestyle guidance 674 24.24 70.43% Medication reminders and management 565 20.32 59.04% Appointment scheduling and queue management 461 16.58 48.17% Education and training resources 295 10.61 30.83% Other 83 2.99 8.67% Total 2780 100 290.49% -
[1] Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int, 2024; 105(4s): S117-S314. doi: 10.1016/j.kint.2023.10.018 [2] Kovesdy C P. Epidemiology of chronic kidney disease: an update 2022. Kidney Int Suppl, 2022; 12(1): 7-11. doi: 10.1016/j.kisu.2021.11.003 [3] Matsushita K, van der Velde M, Astor B C, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet, 2010; 375(9731): 2073-2081. doi: 10.1016/S0140-6736(10)60674-5 [4] Wang K, Liu Q, Tang M, et al. Chronic kidney disease-induced muscle atrophy: molecular mechanisms and promising therapies. Biochem Pharmacol, 2023; 208: 115407. doi: 10.1016/j.bcp.2022.115407 [5] Foreman K J, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet, 2018; 392(10159): 2052-2090. doi: 10.1016/S0140-6736(18)31694-5 [6] Wang L, Xu X, Zhang M, et al. Prevalence of chronic kidney disease in china: results from the sixth China chronic disease and risk factor surveillance. JAMA, 2023; 183(4): 298-310. doi: 10.1001/jamainternmed.2022.6817 [7] GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, 2020; 395(10225): 709-733. doi: 10.1016/S0140-6736(19)32977-0 [8] Bodenheimer T, Wagner E H, Grumbach K. Improving primary care for patients with chronic illness. JAMA, 2002; 288(14): 1775-1779. doi: 10.1001/jama.288.14.1775 [9] Tong A, Chando S, Crowe S, et al. Research priority setting in kidney disease: a systematic review. Am J Kidney Dis, 2015; 65(5): 674-683. doi: 10.1053/j.ajkd.2014.11.011 [10] Donald M, Beanlands H, Straus S, et al. An eHealth self-management intervention for adults with chronic kidney disease, My Kidneys My Health: a mixed-methods study. CMAJ Open, 2022; 10(3): E746-e754. doi: 10.9778/cmajo.20210332 [11] Goodall T A, Halford W K. Self-management of diabetes mellitus: a critical review. Health Psychol, 1991; 10(1): 1-8. doi: 10.1037//0278-6133.10.1.1 [12] Chen R S, Kang E S, Wu L Z, et al. [Cold and Arid Regions Environmental and Engineering Research Institute]. Journal of Glaciology and Geocryology, 2005; 27(4): 469-475. [13] He L, Xue B, Wang B, et al. Impact of high, low, and non-optimum temperatures on chronic kidney disease in a changing climate, 1990-2019: a global analysis. Environ Res, 2022; 212(Pt A): 113172. doi: 10.1016/j.envres.2022.113172 [14] Wei X R, Wang Y C. Contemporary understanding of the risk factors for chronic kidney disease in cold area. Frigid Zone Medicine, 2022; 2(4): 204-213. doi: 10.2478/fzm-2022-0028 [15] Elliott M J, Harrison T G, Love S, et al. Peer support interventions for people with CKD: a scoping review. Am J Kidney Dis, 2025; 85(1): 78-88. doi: 10.1053/j.ajkd.2024.07.007 [16] Shen H, van der Kleij R, van der Boog P J M, et al. Digital tools/eHealth to support CKD self-management: a qualitative study of perceptions, attitudes and needs of patients and health care professionals in China. Int J Med Inform, 2022; 165: 104811. doi: 10.1016/j.ijmedinf.2022.104811 [17] von Elm E, Altman D G, Egger M, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ, 2007; 335(7624): 806-808. doi: 10.1136/bmj.39335.541782.AD [18] Wallston K A, Rothman R L, Cherrington A. Psychometric properties of the Perceived Diabetes Self-Management Scale (PDSMS). J Behav Med, 2007; 30(5): 395-401. doi: 10.1007/s10865-007-9110-y [19] Chew L D, Bradley K A, Boyko E J. Brief questions to identify patients with inadequate health literacy. Fam Med, 2004; 36(8): 588-594. [20] Toobert D J, Hampson S E, Glasgow R E. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care, 2000; 23(7): 943-950. doi: 10.2337/diacare.23.7.943 [21] Wei X R, Jiang R, Liu Y, et al. The effects of cold region meteorology and specific environment on the number of hospital admissions for chronic kidney disease: an investigate with a distributed lag nonlinear model. Frigid Zone Medicine, 2023, 3(2): 65-76. [22] Chatzi A, Doody O. The one-way ANOVA test explained. Nurse Res, 2023; 31(3): 8-14. doi: 10.7748/nr.2023.e1885 [23] Aslam M. Chi-square test under indeterminacy: an application using pulse count data. BMC Med Res Methodol, 2021; 21(1): 201. doi: 10.1186/s12874-021-01400-z [24] Xu W, Li C, Qian G, et al. Association of metabolic syndrome with chronic kidney disease in premenopausal and postmenopausal women. Nan fang yi ke da xue xue bao, 2019; 39(7): 861-866. [25] Zhang L, Zhao M H, Zuo L, et al. China Kidney Disease Network (CK-NET) 2016 Annual Data Report. Kidney Int Suppl, 2020; 10(2): e97-e185. doi: 10.1016/j.kisu.2020.09.001 [26] He L Q, Wu X H, Huang Y Q, et al. Dietary patterns and chronic kidney disease risk: a systematic review and updated meta-analysis of observational studies. Nutr J, 2021; 20(1): 4. doi: 10.1186/s12937-020-00661-6 [27] Masood S, Mashhadi S F, Kazmi S, et al. Self-management in chronic kidney disease patients in a tertiary care hospital in rawalpindi: a cross-sectional study. Pak J Med Res, 2022; 61(2): 79-83. [28] Curtin R B, Walters B A J, Schatell D, et al. Self-efficacy and self-management behaviors in patients with chronic kidney disease. Adv Chronic Kidney Dis, 2008; 15(2): 191-205. doi: 10.1053/j.ackd.2008.01.006 [29] Jiang Y, Zhang C, Hong J, et al. Relationships of person-related, problem-related, and environment-related factors to self-care behaviours and the mediating role of self-confidence among patients with heart failure: Cross-sectional analysis of structural equation modelling. Int J Nurs Stud, 2023; 147: 104590. doi: 10.1016/j.ijnurstu.2023.104590 [30] Ganguli M, Hughes T F, Jia Y, et al. Aging and functional health literacy: a population-based study. Am J Geriatr Psychiatry, 2021; 29(9): 972-981. doi: 10.1016/j.jagp.2020.12.007 [31] Romanova A, Rubinelli S, Diviani N. Improving health and scientific literacy in disadvantaged groups: a scoping review of interventions. Patient Educ Couns, 2024; 122: 108168. doi: 10.1016/j.pec.2024.108168 [32] Hostetter T H, Lising M. National kidney disease education program. J Am Soc Nephrol, 2003; 14(7 Suppl 2): S114-S116. doi: 10.1097/01.ASN.0000070156.78824.C7 [33] Ford E, Stewart K, Garcia E, et al. Randomized Controlled trial of the effect of an exercise rehabilitation program on symptom burden in maintenance hemodialysis: a clinical research protocol. Can J Kidney Health Dis, 2024; 11: 20543581241234724. doi: 10.1177/20543581241234724 [34] Notaras S, Lambert K, Perz J, et al. Diet in the management of non-dialysis dependent chronic kidney disease: perceptions and practices of health professionals. BMC Nephrol, 2022; 23(1): 158. doi: 10.1186/s12882-022-02790-y [35] Aguiar M, Trujillo M, Chaves D, et al. mHealth apps using behavior change techniques to self-report data: systematic review. JMIR MHealth UHealth, 2022; 10(9): e33247. doi: 10.2196/33247 [36] Kalaitzaki A, Rovithis M, Dimitropoulos A, et al. Promoting self-management and independent living of older individuals with chronic diseases through technology: a study of self-reported needs, priorities, and preferences. Medicina (Kaunas), 2023; 59(8): 1493. doi: 10.3390/medicina59081493 [37] Shaw G, Whelan M E, Armitage L C, et al. Are COPD self-management mobile applications effective? A systematic review and meta-analysis. NPJ Prim Care Respir Med, 2020; 30(1): 11. doi: 10.1038/s41533-020-0167-1 [38] Bekfani T, Fudim M, Cleland J G F, et al. A current and future outlook on upcoming technologies in remote monitoring of patients with heart failure. Eur J Heart Fail, 2021; 23(1): 175-185. doi: 10.1002/ejhf.2033 [39] Meacock R, Anselmi L, Kristensen S R, et al. Do variations in hospital admission rates bias comparisons of standardized hospital mortality rates? A population-based cohort study. Soc Sci Med, 2019; 235: 112409. doi: 10.1016/j.socscimed.2019.112409 [40] Lieb M, Hepp T, Schiffer M, et al. Accuracy and concordance of measurement methods to assess non-adherence after renal transplantation-a prospective study. BMC Nephrol, 2020; 21(1): 114. doi: 10.1186/s12882-020-01781-1 -


 投稿系统
投稿系统


 下载:
下载: