The impact of low ambient temperature on cardiovascular health
doi: 10.2478/fzm-2023-0021
-
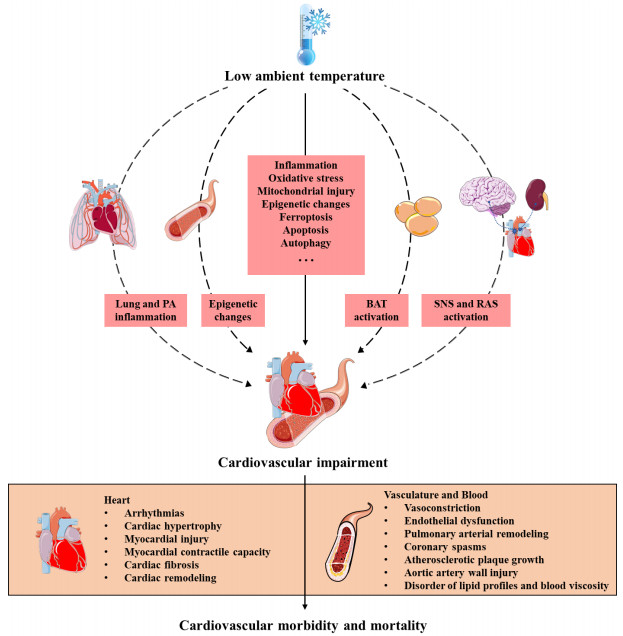
Abstract: Extreme weather events and climate change have witnessed a substantial increase in recent years, leading to heightened concerns. The rise in abnormal ambient temperatures, both in intensity and frequency, directly and indirectly impacts cardiovascular health. While the impact of high ambient temperatures on cardiovascular response is a common concern in the context of global warming, the significance of low temperatures cannot be overlooked. The challenges posed by low temperatures contribute to increased cardiovascular morbidity and mortality, posing a significant threat to global public health. This review aims to provide an overview of the relationship between low ambient temperature and cardiovascular health, encompassing the burden of cardiovascular outcomes and underlying mechanisms. Additionally, the review explores strategies for cold adaptation and cardioprotection. We posit that to optimize cold adaptation strategies, future research should delve deeper into the underlying mechanisms of cardiovascular health in response to low ambient temperature exposure.
-
Key words:
- low ambient temperature /
- cardiovascular health /
- cold adaptation
-
Table 1. Summary of selected studies on low ambient temperature and CVD mortality
Authors (year of publication) Study region Study period Population size Outcome variables Main outcome Reference Carder et al. (2005) 3 large cities in Scottish 1981–2001 1, 652, 000 Cardiorespiratory mortality For temperatures below 11℃, a 1℃ drop in the daytime mean temperature on any day was associated with an increase in mortality of 3.4% (95% CI: 2.6, 4.1) over the following month for CVD disease. [47] Zeka et al. (2014) Ireland 1984–2007 1, 057, 046 CVD mortality CVD mortality showed the greatest increase associated with temperatures in the preceding week; the impact of cold temperature on mortality was slightly weakened, but lasted up to 4 weeks prior to death. [49] Wang et al. (2015) Beijing and Shanghai, China 2007–2009 none CVD mortality People with hypertensive disease were particularly susceptible to extremely low temperature in Beijing. People with ischemic heart disease in Shanghai showed greater susceptibility to extremely cold temperature. [48] Yang et al. (2015) 15 cities in China 2007–2013 1, 936, 116 CVD mortality Cold weather was responsible for temperature-related CVD death burden with a fraction of 15.8% (95% CI: 13.1%, 17.9%), corresponding to 305902 deaths. [34] Zhang et al. (2016) Wuhan, China 2003–2010 32, 721 CVD mortality For cold effects over lag 0–21 days, a 1℃ decrease in mean temperature below the cold thresholds was associated with a 3.65% (95% CI: 2.62, 4.69) increase in CVD mortality. [46] Fu et al. (2018) India 2001–2013 40, 003 Ischemic heart disease death Moderately cold temperature (13.8℃) was estimated to have higher attributable risks (9.7% [95% CI: 3.7, 15.3]) for ischemic heart disease death than extreme cold one. [38] Zhang et al. (2018) Yinchuan, China 2010–2015 26, 097 CVD mortality Cold temperature was associated with significantly delayed CVD mortality. [27] Chen et al. (2018) 272 main Chinese cities 2013–2015 1, 826, 186 CVD mortality Compared to the minimum mortality temperatures, extreme cold temperature had larger relative risks (1.92 [95% CI: 1.75, 2.10]) than extreme hot temperature (RR: 1.22 [95% CI: 1.16, 1.28]) on CVD mortality. [23] Lv et al. (2020) Hunan, China 2013–2017 none YLL rate Cold temperature was responsible for most of the YLL for cardiovascular death, with an overall estimate of 15.94% (8.82%, 23.05%). [43] Cheng et al. (2021) Hong Kong, China 2000–2016 67, 157 YLL Cold was estimated to cause life expectancy loss of 0.9 years in total cardiovascular disease. [41] Hu et al. (2021) 364 locations across China 2006–2017 none YLL An average of 1.07 (95% CI: 1.00, 1.15) years life loss per CVD death was associated with cold temperature. [26] Liu et al. (2021) 364 locations across China 2013–2017 none YLL rate A mean of 1.1 (95% CI: 0.67, 1.37) YLL per CVD death was attributable to cold temperature. [44] Lv et al. (2022) Hunan, China 2013–2017 711, 484 YLL rates Life loss per death of cardiovascular diseases attributable to cold temperature was 1.13 (95% CI: 0.89, 1.37), particularly moderate cold (1.00, 95% CI: 0.78, 1.23). [19] Xu et al. (2022) Jiangsu, China 2015–2019 1, 000, 014 CVD mortality Exposure to extreme cold (−0.6℃) was significantly associated with increased odds of mortality (1.79, 95% CI: 1.73, 1.85). [20] CVD, cardiovascular disease; CI, confidence interval; eCI, empirical confidence interval; RR, relative risk; YLL, years of life lost. Table 2. Summary of selected studies on low ambient temperature and CVD morbidity
Authors (year of publication) Study region Study period Population size Outcome variables Main outcome Reference Sartini et al. (2016) British 1998–2012 none CVD morbidity CVD risks were higher in winter. [55] Bai et al. (2016) Ontario, Canada 1996–2013 395, 840 Hospitalizations from hypertensive diseases and arrhythmia Compared to the temperature with minimum risk of morbidity, cold temperatures (1st percentile) were associated with a 37% (95% CI: 5%, 78%) increase in hypertension-related hospitalizations. Arrhythmia was not linked to temperatures. [32] Hensel et al. (2017) Hamburg, Germany 2010–2014 510, 389 CVD emergencies Coronary artery disease, cardiac pulmonary edema and hypertensive urgency were increased at low temperatures, particularly below 10℃. [33] Ponjoan et al. (2017) Catalan 2006–2013 22, 611 CVD emergency hospitalization The overall incidence of CVD hospitalization was significantly increased during cold spells (IRR = 1.120; 95% CI: 1.10, 1.30) and the effect was even stronger in the 7 days subsequent to the cold spell (IRR = 1.29; 95% CI: 1.22, 1.36). [59] Bai et al. (2018) Ontario, Canada 1996–2013 1, 389, 057 Coronary heart disease hospitalization On cold days with temperature corresponding to the 1st percentile of temperature distribution, a 9% increase in daily hospitalizations for coronary heart disease (95% CI: 1%, 16%), 29% increase for myocardial infarction (95% CI: 15%, 45%) and 11% increase for stroke (95% CI: 1%, 22%) relative to the days with an optimal temperature. [29] Zhao et al. (2018) Ningxia, China 2012–2015 158, 733 Clinical visit Cold effect on cardiovascular visits appeared at the lag 6th day and persisted until the 22nd day, resulting in a cumulative relative risk (RR) 1.55 (95% CI: 1.26, 1.92), compared to the minimum-clinical visit temperature. [40] Liu et al. (2018) Beijing, China 2013–2016 81, 029 Acute myocardial infarction (AMI) hospitalization Compared to the 10th percentile temperature measured by daily mean temperature (T mean), daily minimum temperature (T min) and daily minimum apparent temperature (AT min), the cumulative RR at 1st percentile of T mean, T min and AT min for AMI hospitalization were 1.15 (95% CI: 1.02, 1.30), 1.24 (95% CI: 1.11, 1.38) and 1.41 (95% CI: 1.18, 1.68), respectively. [51] Mohammadi et al. (2018) Tehran, Iran 2013–2016 15, 835 AMI hospitalization Cold temperatures increased the risk of AMI admissions. [53] Xu et al. (2019) Suzhou, China 2013–2016 100 Blood pressure The systolic blood pressure, diastolic blood pressure, pulse pressure, and mean arterial pressure decreased with hourly temperature decreased. [56] Cui et al. (2019) Hefei, China 2015–2017 35, 096 Hospital admission Compared to the 25th percentile of temperature (10.3℃), the cumulative RR of extremely low temperature (1st percentile of temperature, 0.075℃) over lag 0–27 days was 0.616 (95% CI: 0.423, 0.891), and the cumulative RR of moderate low temperature (10th percentile of temperature, 5.16℃) was 1.081 (95% CI: 1.019, 1.147) over lag 0–7 days. [54] Tian et al. (2020) Hong Kong, China 2005–2012 521, 575 Emergency CVD hospitalization Compared to the identified optimal temperature at 23.0℃, the cumulative relative risk during 0 to 21 lag days was 1.69 (95% CI: 1.56, 1.82) for extreme cold (1st percentile) and 1.22 (95% CI: 1.15, 1.29) for moderate cold temperature (10th percentile). [39] Kang et al. (2020) 31 provinces in China 2012–2015 451, 770 Blood pressure An overall 10℃ decrease in ambient temperature was statistically associated with 0.74 mmHg (95% CI: 0.69, 0.79) and 0.60 mmHg (95% CI: −0.63, −0.57) rise in systolic and diastolic blood pressure, respectively. [52] Lavigne et al. (2021) Toronto, Canada 2002–2010 292, 666 CVD morbidity The effect of extreme cold temperatures (1st percentile of temperature distribution vs. 25th percentile) on CVD emergency room visits was stronger for individuals with comorbid cardiac (REM = 1.47; 95% CI: 1.06, 2.23) and kidney diseases (REM = 2.43; 95% CI: 1.59, 8.83). [58] Fonseca-Rodríguez et al. (2021) Sweden 1991–2014 1, 630, 189 CVD hospitalization Moist and very cold weather was related to a delayed increase in cardiovascular hospitalizations. [21] CVD, cardiovascular disease; CI, confidence interval; RR, relative risk; YLL, years of life lost; IRR, Incidence rate ratios; REM, relative effect modification. -
[1] Romanello M, McGushin A, Di Napoli C, et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet, 2021; 398(10311): 1619–1662. doi: 10.1016/S0140-6736(21)01787-6 [2] Cai W, Zhang C, Zhang S, et al. The 2021 China report of the Lancet Countdown on health and climate change: seizing the window of opportunity. Lancet Public Health, 2021; 6(12): e932–e947. doi: 10.1016/S2468-2667(21)00209-7 [3] Romanello M, van Daalen K, Anto J M, et al. Tracking progress on health and climate change in Europe. Lancet Public Health, 2021; 6(11): e858–e865. doi: 10.1016/S2468-2667(21)00207-3 [4] Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet, 2021; 397(10269): 129–170. doi: 10.1016/S0140-6736(20)32290-X [5] Ebi K L, Vanos J, Baldwin J W, et al. Extreme weather and climate change: Population health and health system implications. Annu Rev Public Health, 2021; 42: 293–315. doi: 10.1146/annurev-publhealth-012420-105026 [6] Kotcher J, Maibach E, Miller J, et al. Views of health professionals on climate change and health: a multinational survey study. Lancet Planet Health, 2021; 5(5): e316–e323. doi: 10.1016/S2542-5196(21)00053-X [7] Johnson N C, Xie S P, Kosaka Y, et al. Increasing occurrence of cold and warm extremes during the recent global warming slowdown. Nat Commun, 2018; 9(1): 1724. doi: 10.1038/s41467-018-04040-y [8] Wang C, Yao Y, Wang H, et al. The 2020 summer floods and 2020/21 winter extreme cold surges in China and the 2020 typhoon season in the Western North Pacific. Adv Atmos Sci, 2021; 38(6): 896–904. doi: 10.1007/s00376-021-1094-y [9] He Q, Silliman B R. Climate change, human impacts, and coastal ecosystems in the anthropocene. Curr Biol, 2019; 29(19): R1021–R1035. doi: 10.1016/j.cub.2019.08.042 [10] Song X, Wang S, Hu Y, et al. Impact of ambient temperature on morbidity and mortality: An overview of reviews. Sci Total Environ, 2017; 586: 241–254. doi: 10.1016/j.scitotenv.2017.01.212 [11] Argacha J F, Bourdrel T, van de Borne P. Ecology of the cardiovascular system: A focus on air-related environmental factors. Trends Cardiovasc Med, 2018; 28(2): 112–126. doi: 10.1016/j.tcm.2017.07.013 [12] Liu C Q, Yavar Z B, Sun Q H. Cardiovascular response to thermoregulatory challenges. Am J Physiol Heart Circ Physiol, 2015; 309(11): H1793–H1812. doi: 10.1152/ajpheart.00199.2015 [13] Chen J M, Gao Y, Jiang Y X, et al. Low ambient temperature and temperature drop between neighbouring days and acute aortic dissection: a case-crossover study. European Heart Journal, 2022; 43(3): 228–235. doi: 10.1093/eurheartj/ehab803 [14] Ciuha U, Sotiridis A, Mlinar T, et al. Heat acclimation enhances the cold-induced vasodilation response. Eur J Appl Physiol, 2021; 121(11): 3005–3015. doi: 10.1007/s00421-021-04761-x [15] Chen C W, Wu C H, Liou Y S, et al. Roles of cardiovascular autonomic regulation and sleep patterns in high blood pressure induced by mild cold exposure in rats. Hypertens Res, 2021; 44(6): 662–673. doi: 10.1038/s41440-021-00619-z [16] Umishio W, Ikaga T, Kario K, et al. Electrocardiogram abnormalities in residents in cold homes: a cross-sectional analysis of the nationwide Smart Wellness Housing survey in Japan. Environ Health Prev Med, 2021; 26(1): 104. doi: 10.1186/s12199-021-01024-1 [17] Bai L, Cirendunzhu, Woodward A, et al. Temperature and mortality on the roof of the world: a time-series analysis in three Tibetan counties, China. Sci Total Environ, 2014; 485–486: 41–48. [18] Wang B, Chai G R, Sha Y Z, et al. Association between ambient temperature and cardiovascular disease hospitalisations among farmers in suburban northwest China. Int J Biometeorol, 2022; 66(7): 1317–1327. doi: 10.1007/s00484-022-02278-2 [19] Lv L S, Zhou C L, Jin D H, et al. Impact of ambient temperature on life loss per death from cardiovascular diseases: a multicenter study in central China. Environ Sci Pollut Res Int, 2022; 29(11): 15791–15799. doi: 10.1007/s11356-021-16888-7 [20] Xu R, Shi C, Wei J, et al. Cause-specific cardiovascular disease mortality attributable to ambient temperature: A time-stratified case-crossover study in Jiangsu province, China. Ecotoxicol Environ Saf, 2022; 236: 113498. doi: 10.1016/j.ecoenv.2022.113498 [21] Fonseca-Rodriguez O, Sheridan S C, Lundevaller E H, et al. Effect of extreme hot and cold weather on cause-specific hospitalizations in Sweden: A time series analysis. Environ Res, 2021; 193: 110535. doi: 10.1016/j.envres.2020.110535 [22] Wang Q, Li C, Guo Y, et al. Environmental ambient temperature and blood pressure in adults: A systematic review and meta-analysis. Sci Total Environ; 2017; 575: 276–286. doi: 10.1016/j.scitotenv.2016.10.019 [23] Chen R J, Yin P, Wang L J, et al. Association between ambient temperature and mortality risk and burden: time series study in 272 main Chinese cities. BMJ, 2018; 363: k4306. [24] Denpetkul T, Phosri A. Daily ambient temperature and mortality in Thailand: Estimated effects, attributable risks, and effect modifications by greenness. Sci Total Environ. 2021; 791: 148373. doi: 10.1016/j.scitotenv.2021.148373 [25] Lin Y K, Sung F C, Honda Y, et al. Comparative assessments of mortality from and morbidity of circulatory diseases in association with extreme temperatures. Sci Total Environ, 2020; 723: 138012. doi: 10.1016/j.scitotenv.2020.138012 [26] Hu J, Hou Z, Xu Y, et al. Life loss of cardiovascular diseases per death attributable to ambient temperature: A national time series analysis based on 364 locations in China. Sci Total Environ, 2021; 756: 142614. doi: 10.1016/j.scitotenv.2020.142614 [27] Zhang H, Wang Q, Zhang Y, et al. Modeling the impacts of ambient temperatures on cardiovascular mortality in Yinchuan: evidence from a northwestern city of China. Environ Sci Pollut Res Int, 2018; 25(6): 6036–6043. doi: 10.1007/s11356-017-0920-3 [28] Hurtado-Diaz M, Cruz J C, Texcalac-Sangrador J L, et al. Short-term effects of ambient temperature on non-external and cardiovascular mortality among older adults of metropolitan areas of Mexico. Int J Biometeorol, 2019; 63(12): 1641–1650. doi: 10.1007/s00484-019-01778-y [29] Bai L, Li Q, Wang J, et al. Increased coronary heart disease and stroke hospitalisations from ambient temperatures in Ontario. Heart, 2018; 104(8): 673–679. doi: 10.1136/heartjnl-2017-311821 [30] Macintyre H L, Heaviside C, Cai X M, et al. The winter urban heat island: Impacts on cold-related mortality in a highly urbanized European region for present and future climate. Environ Int, 2021; 154: 106530. doi: 10.1016/j.envint.2021.106530 [31] Xu E, Li Y N, Li T T, et al. Association between ambient temperature and ambulance dispatch: a systematic review and meta-analysis. Environ Sci Pollut Res Int, 2022; 29(44): 66335–66347. doi: 10.1007/s11356-022-20508-3 [32] Bai L, Li Q, Wang J, et al. Hospitalizations from hypertensive diseases, diabetes, and arrhythmia in relation to low and high temperatures: Population-based study. Sci Rep, 2016; 6: 30283. doi: 10.1038/srep30283 [33] Hensel M, Stuhr M, Geppert D, et al. Relationship between ambient temperature and frequency and severity of cardiovascular emergencies: A prospective observational study based on out-of-hospital care data. Int J Cardiol, 2017; 228: 553–557. doi: 10.1016/j.ijcard.2016.11.155 [34] Yang J, Yin P, Zhou M, et al. Cardiovascular mortality risk attributable to ambient temperature in China. Heart, 2015; 101(24): 1966–1972. doi: 10.1136/heartjnl-2015-308062 [35] Luo Q L, Li S S, Guo Y M, et al. A systematic review and meta-analysis of the association between daily mean temperature and mortality in China. Environ Res, 2019; 173: 281–299. doi: 10.1016/j.envres.2019.03.044 [36] Wichmann J, Andersen Z, Ketzel M, et al. Apparent temperature and cause-specific emergency hospital admissions in Greater Copenhagen, Denmark. PLoS One, 2011; 6(7): e22904. doi: 10.1371/journal.pone.0022904 [37] Phung D, Thai P K, Guo Y, et al. Ambient temperature and risk of cardiovascular hospitalization: An updated systematic review and meta-analysis. Sci Total Environ, 2016; 550: 1084–1102. doi: 10.1016/j.scitotenv.2016.01.154 [38] Fu S H, Gasparrini A, Rodriguez P S, et al. Mortality attributable to hot and cold ambient temperatures in India: a nationally representative case-crossover study. PLoS Med, 2018; 15(7): e1002619. doi: 10.1371/journal.pmed.1002619 [39] Tian L W, Qiu H, Sun S Z, et al. Emergency cardiovascular hospitalization risk attributable to cold temperatures in Hong Kong. Circ Cardiovasc Qual Outcomes, 2016; 9(2): 135–142. doi: 10.1161/CIRCOUTCOMES.115.002410 [40] Zhao Q, Zhao Y, Li S, et al. Impact of ambient temperature on clinical visits for cardio-respiratory diseases in rural villages in northwest China. Sci Total Environ, 2018; 612: 379–385. doi: 10.1016/j.scitotenv.2017.08.244 [41] Cheng J, Ho H C, Su H, et al. Low ambient temperature shortened life expectancy in Hong Kong: A time-series analysis of 1.4 million years of life lost from cardiorespiratory diseases. Environ Res, 2021; 201: 111652. doi: 10.1016/j.envres.2021.111652 [42] Li H, Yao Y, Duan Y, et al. Years of life lost and mortality risk attributable to non-optimum temperature in Shenzhen: a time-series study. J Expo Sci Environ Epidemiol, 2021; 31(1): 187–196. doi: 10.1038/s41370-020-0202-x [43] Lv L S, Jin D H, Ma W J, et al. The impact of non-optimum ambient temperature on years of life lost: A multi-county observational study in Hunan, China. Int J Environ Res Public Health, 2020; 17(11): 3810. doi: 10.3390/ijerph17113810 [44] Liu T, Zhou C, Zhang H, et al. Ambient temperature and years of life lost: A national study in China. Innovation (Camb), 2021; 2(1): 100072. [45] Luan G, Yin P, Li T, et al. The years of life lost on cardiovascular disease attributable to ambient temperature in China. Sci Rep, 2017; 7(1): 13531. doi: 10.1038/s41598-017-13225-2 [46] Zhang Y Q, Li C L, Feng R J, et al. The short-term effect of ambient temperature on mortality in Wuhan, China: A time-series study using a distributed lag non-linear model. Int J Environ Res Public Health, 2016; 13(7): 722. doi: 10.3390/ijerph13070722 [47] Carder M, McNamee R, Beverland I, et al. The lagged effect of cold temperature and wind chill on cardiorespiratory mortality in Scotland. Occup Environ Med, 2005; 62(10): 702–710. doi: 10.1136/oem.2004.016394 [48] Wang X, Li G, Liu L, et al. Effects of extreme temperatures on cause-specific cardiovascular mortality in China. Int J Environ Res Public Health, 2015; 12(12): 16136–16156. doi: 10.3390/ijerph121215042 [49] Zeka A, Browne S, McAvoy H, et al. The association of cold weather and all-cause and cause-specific mortality in the island of Ireland between 1984 and 2007. Environ Health, 2014; 13: 104. doi: 10.1186/1476-069X-13-104 [50] Bunker A, Wildenhain J, Vandenbergh A, et al. Effects of air temperature on climate-sensitive mortality and morbidity outcomes in the elderly; A systematic review and meta-analysis of epidemiological evidence. EBioMedicine, 2016; 6: 258–268. doi: 10.1016/j.ebiom.2016.02.034 [51] Liu X L, Kong D H, Fu J, et al. Association between extreme temperature and acute myocardial infarction hospital admissions in Beijing, China: 2013–2016. Plos One, 2018; 13(10): e0204706. doi: 10.1371/journal.pone.0204706 [52] Kang Y, Han Y, Guan T, et al. Clinical blood pressure responses to daily ambient temperature exposure in China: An analysis based on a representative nationwide population. Sci Total Environ, 2020; 705: 135762. doi: 10.1016/j.scitotenv.2019.135762 [53] Mohammadi R, Soori H, Alipour A, et al. The impact of ambient temperature on acute myocardial infarction admissions in Tehran, Iran. J Therm Biol, 2018; 73: 24–31. doi: 10.1016/j.jtherbio.2018.02.008 [54] Cui L, Geng X, Ding T, et al. Impact of ambient temperature on hospital admissions for cardiovascular disease in Hefei City, China. Int J Biometeorol, 2019; 63(6): 723–734. doi: 10.1007/s00484-019-01687-0 [55] Sartini C, Barry S J E, Wannamethee S G, et al. Effect of cold spells and their modifiers on cardiovascular disease events: Evidence from two prospective studies. Int J Cardiol, 2016; 218: 275–283. doi: 10.1016/j.ijcard.2016.05.012 [56] Xu D, Zhang Y, Wang B, et al. Acute effects of temperature exposure on blood pressure: An hourly level panel study. Environ Int, 2019; 124: 493–500. doi: 10.1016/j.envint.2019.01.045 [57] Masajtis-Zagajewska A, Pawlowicz E, Nowicki M. Effect of short-term cold exposure on central aortic blood pressure in patients with CKD. Nephron, 2021; 145(1): 20–26. doi: 10.1159/000510365 [58] Lavigne E, Gasparrini A, Wang X, et al. Extreme ambient temperatures and cardiorespiratory emergency room visits: assessing risk by comorbid health conditions in a time series study. Environ Health, 2014; 13(1): 5. doi: 10.1186/1476-069X-13-5 [59] Ponjoan A, Blanch J, Alves-Cabratosa L, et al. Effects of extreme temperatures on cardiovascular emergency hospitalizations in a Mediterranean region: a self-controlled case series study. Environ Health, 2017; 16(1): 32. doi: 10.1186/s12940-017-0238-0 [60] Zhang J, Chen R, Zhang G, et al. PM2.5 increases mouse blood pressure by activating toll-like receptor 3. Ecotoxicol Environ Saf, 2022; 234: 113368. doi: 10.1016/j.ecoenv.2022.113368 [61] Kim S R, Choi S, Kim K, et al. Association of the combined effects of air pollution and changes in physical activity with cardiovascular disease in young adults. Eur Heart J, 2021; 42(25): 2487–2497. doi: 10.1093/eurheartj/ehab139 [62] Klompmaker J O, Hart J E, James P, et al. Air pollution and cardiovascular disease hospitalization - Are associations modified by greenness, temperature and humidity? Environ Int, 2021; 156: 106715. doi: 10.1016/j.envint.2021.106715 [63] Hsu W H, Hwang S A, Kinney P L, et al. Seasonal and temperature modifications of the association between fine particulate air pollution and cardiovascular hospitalization in New York state. Sci Total Environ, 2017; 578: 626–632. doi: 10.1016/j.scitotenv.2016.11.008 [64] Luo B, Zhang S, Ma S, et al. Effects of cold air on cardiovascular disease risk factors in rat. Int J Environ Res Public Health, 2012; 9(7): 2312–2325. doi: 10.3390/ijerph9072312 [65] Zhang X K, Zhang S Y, Wang C L, et al. Effects of moderate strength cold air exposure on blood pressure and biochemical indicators among cardiovascular and cerebrovascular patients. Int J Environ Res Public Health, 2014; 11(3): 2472–2487. doi: 10.3390/ijerph110302472 [66] Greaney J L, Kenney W L, Alexander L M. Sympathetic function during whole body cooling is altered in hypertensive adults. Journal of Applied Physiology, 2017; 123(6): 1617–1624. doi: 10.1152/japplphysiol.00613.2017 [67] Claeys M J, Rajagopalan S, Nawrot T S, et al. Climate and environmental triggers of acute myocardial infarction. Eur Heart J, 2017: 38(13): 955–960. [68] Okamoto-Mizuno K, Tsuzuki K, Mizuno K, et al. Effects of low ambient temperature on heart rate variability during sleep in humans. Eur J Appl Physiol, 2009; 105(2): 191–197. doi: 10.1007/s00421-008-0889-1 [69] Thu Dang T A, Wraith D, Bambrick H, et al. Short - term effects of temperature on hospital admissions for acute myocardial infarction: A comparison between two neighboring climate zones in Vietnam. Environ Res, 2019;: 175: 167–177. doi: 10.1016/j.envres.2019.04.023 [70] Lim Y H, Park M S, Kim Y, et al. Effects of cold and hot temperature on dehydration: a mechanism of cardiovascular burden. Int J Biometeorol, 2015; 59(8): 1035–1043. doi: 10.1007/s00484-014-0917-2 [71] Li H, Yue P, Su Y, et al. Plasma levels of matrix metalloproteinase-9: A possible marker for cold-induced stroke risk in hypertensive rats. Neurosci Lett, 2019; 709: 134399. doi: 10.1016/j.neulet.2019.134399 [72] Luo B, Zhang S Y, Ma S C, et al. Artificial cold air increases the cardiovascular risks in spontaneously hypertensive rats. Int J Environ Res Public Health, 2012; 9(9): 3197–3208. doi: 10.3390/ijerph9093197 [73] Ebner A, Poitz D M, Alexiou K, et al. Secretion of adiponectin from mouse aorta and its role in cold storage-induced vascular dysfunction. Basic Res Cardiol, 2013; 108(6): 390. doi: 10.1007/s00395-013-0390-9 [74] Crosswhite P, Chen K, Sun Z. AAV delivery of tumor necrosis factor-alpha short hairpin RNA attenuates cold-induced pulmonary hypertension and pulmonary arterial remodeling. Hypertension, 2014; 64(5): 1141–1150. doi: 10.1161/HYPERTENSIONAHA.114.03791 [75] Yin K, Zhao L, Feng D, et al. Resveratrol attenuated low ambient temperature-induced myocardial hypertrophy via inhibiting cardiomyocyte apoptosis. Cell Physiol Biochem, 2015; 35(6): 2451–2462. doi: 10.1159/000374045 [76] Dong M, Yang X, Lim S, et al. Cold exposure promotes atherosclerotic plaque growth and instability via UCP1-dependent lipolysis. Cell Metab, 2013; 18(1): 118–129. doi: 10.1016/j.cmet.2013.06.003 [77] Williams J W, Elvington A, Ivanov S, et al. Thermoneutrality but not UCP1 deficiency suppresses monocyte mobilization into blood. Circ Res, 2017; 121(6): 662–676. doi: 10.1161/CIRCRESAHA.117.311519 [78] Xue Y, Yu X, Zhang X, et al. Protective effects of ginsenoside Rc against acute cold exposure-induced myocardial injury in rats. J Food Sci, 2021; 86(7): 3252–3264. doi: 10.1111/1750-3841.15757 [79] Cong P, Liu Y, Liu N, et al. Cold exposure induced oxidative stress and apoptosis in the myocardium by inhibiting the Nrf2-Keap1 signaling pathway. BMC Cardiovasc Disord, 2018; 18(1): 36. doi: 10.1186/s12872-018-0748-x [80] Park J, Kim S, Kim D H, et al. Whole-body cold tolerance in older Korean female divers "haenyeo" during cold air exposure: effects of repetitive cold exposure and aging. Int J Biometeorol, 2018; 62(4): 543–551. doi: 10.1007/s00484-017-1463-5 [81] Yin Z Q, Ding G B, Chen X, et al. Beclin1 haploinsufficiency rescues low ambient temperature-induced cardiac remodeling and contractile dysfunction through inhibition of ferroptosis and mitochondrial injury. Metabolism, 2020; 113: 154397. doi: 10.1016/j.metabol.2020.154397 [82] Jiang S, Guo R, Zhang Y, et al. Heavy metal scavenger metallothionein mitigates deep hypothermia-induced myocardial contractile anomalies: role of autophagy. Am J Physiol Endocrinol Metab, 2013; 304(1): E74–86. doi: 10.1152/ajpendo.00176.2012 [83] Zhang Y, Li L, Hua Y, et al. Cardiac-specific knockout of ET(A) receptor mitigates low ambient temperature-induced cardiac hypertrophy and contractile dysfunction. J Mol Cell Biol, 2012; 4(2): 97–107. doi: 10.1093/jmcb/mjs002 [84] Zhang Y M, Hu N, Hua Y A, et al. Cardiac over expression of metallothionein rescues cold exposure-induced myocardial contractile dysfunction through attenuation of cardiac fibrosis despite cardiomyocyte mechanical anomalies. Free Radic Biol Med, 2012; 53(2): 194–207. doi: 10.1016/j.freeradbiomed.2012.04.005 [85] Liang J, Yin K, Cao X, et al. Attenuation of low ambient temperature-induced myocardial hypertrophy by atorvastatin via promoting Bcl-2 expression. Cell Physiol Biochem, 2017; 41(1): 286–295. doi: 10.1159/000456111 [86] Chen P G, Sun Z. AAV delivery of endothelin-1 shRNA attenuates cold-induced hypertension. Hum Gene Ther, 2017; 28(2): 190–199. doi: 10.1089/hum.2016.047 [87] Luo Y, Zhang Y, Han X, et al. Akkermansia muciniphila prevents cold-related atrial fibrillation in rats by modulation of TMAO induced cardiac pyroptosis. EbioMedicine, 2022; 82: 104087. doi: 10.1016/j.ebiom.2022.104087 [88] Lu P, Xia G X, Zhao Q, et al. Temporal trends of the association between ambient temperature and hospitalisations for cardiovascular diseases in Queensland, Australia from 1995 to 2016: A time-stratified case-crossover study. Plos Medicine, 2020: 17(7): e1003176. doi: 10.1371/journal.pmed.1003176 [89] Yang C Y, Meng X, Chen R J, et al. Long-term variations in the association between ambient temperature and daily cardiovascular mortality in Shanghai, China. Sci Total Environ, 2015; 538: 524–530. doi: 10.1016/j.scitotenv.2015.08.097 [90] Martinez-Solanas E, Basagana X. Temporal changes in temperature-related mortality in Spain and effect of the implementation of a Heat Health Prevention Plan. Environ Res, 2019; 169: 102–113. doi: 10.1016/j.envres.2018.11.006 [91] Hauton D, May S, Sabharwal R, et al. Cold-impaired cardiac performance in rats is only partially overcome by cold acclimation. J Exp Biol, 2011; 214(18): 3021–3031. doi: 10.1242/jeb.053587 [92] Manolis A S, Manolis S A, Manolis A A, et al. Winter swimming: Body hardening and cardiorespiratory protection via sustainable acclimation. Curr Sports Med Rep, 2019; 18(11): 401–415. doi: 10.1249/JSR.0000000000000653 -


 投稿系统
投稿系统


 下载:
下载: