Pharmacodynamics of frigid zone plant Taxus cuspidata S. et Z. against skin melanin deposition, oxidation, inflammation and allergy
doi: 10.2478/fzm-2023-0007
-
Abstract:
Background Taxus cuspidata S. et Z. is a precious species of frigid zone plant belonging to the Taxaceae family, which possesses anticancer, anti-inflammatory, hypoglycemic, and antibacterial pharmacological properties. While taxane extracted from Taxus chinensis has been reported to elicit antioxidant activities, whether Taxus cuspidata S. et Z. has skin-protective actions against injuries remained unknown. This study aims to explore the pharmacological effects of three Taxus extracts on skin melanin deposition, oxidation, inflammation, and allergy so as to provide new ideas for the prevention and treatment of various diseases related to skin damage. Methods Skin melanin deposition was evaluated by measuring melanin content in the skin of guinea pigs by alkali lysis method. Antioxidant capacity was evaluated by measuring superoxide dismutase (SOD) concentration and glutathione (GSH) content in skin tissue homogenates of Kunming mice by SOD assay kit and micro reduced GSH assay kit. The quantitative real-time polymerase chain reaction (qRT-PCR) and western blotting were used to examine the levels of both SOD and recombinant glutathione peroxidase 4 (GPX4). Skin inflammation was evaluated by xylene-induced ear swelling test and egg-white-induced paw swelling test in mice. In a mouse model of skin allergy induced by 4-aminopyridine (4-AP), allergy was determined by licking body counts and histamine concentrations in tissue homogenates using enzyme-linked immunosorbent assay (ELISA) kits. Two proinflammatory factors tumor necrosis factor (TNF)-α and interleukin (IL)-1β were measured by qRT-PCR. Hematoxylin and eosin (HE) staining was conducted to assess the degree of skin lesion. Results All three Taxus extracts including Taxus chinensis essential oil, Taxus chinensis extract and Taxus chinensis extract compound reduced the melanin deposits in the back skin relative to the non-treated control animals, of which Taxus chinensis essential oil produced the greatest effect. In contrast, the three Taxus extracts elevated SOD and GSH levels in the skin tissues, and the highest increase was seen with Taxus chinensis essential oil. Three Taxus extracts, especially Taxus chinensis essential oil, effectively reduce the rate of ear and paw swelling. All three Taxus extracts reduced the number of body licks, the levels of TNF-α and IL-1β, and the histamine content in tissue homogenates of mice and alleviated skin damage. Consistently, Taxus chinensis essential oil yielded the greatest magnitude of decreases. Conclusion While all three Taxus extracts possessed the anti-skin melanin deposition, oxidation, and allergy properties, Taxus chinensis essential oil produced the superior effects. -
Key words:
- Taxus cuspidata S. et Z. /
- skin melanin deposition /
- oxidation /
- inflammation /
- allergy
-
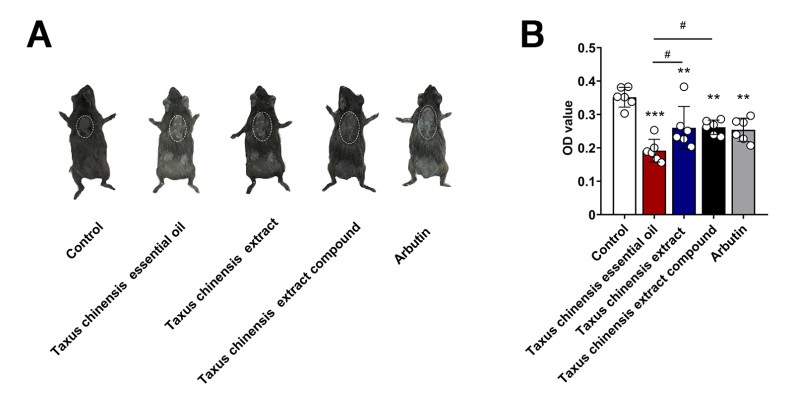
Figure 1. Anti skin melanin deposition effect of three Taxus chinensis extracts (N = 6)
(A) Representative images of guinea pigs in each group after 28 days of administration; (B) Melanin content of back skin of guinea pigs in each group after 28 days of administration; Data represent the mean ± SE; **P < 0.01; ***P < 0.001 vs. Control group; #P < 0.05 vs. Taxus chinensis essential oil group.
Figure 2. Anti skin oxidation effect of three Taxus chinensis extracts (N = 3-5)
(A)Representative images of Kunming mice in each group after 7 days of drug administration; (B) SOD content in the skin tissue homogenates of mice in each group; (C)GSH content of in the skin tissue homogenates of mice in each group; (D) (E) mRNA level of SOD and GPX4 in the skin tissue of each group were tested; (F) Protein relative level of GPX4 in the skin tissue of each group were tested; Data represent the mean ± SE; *P < 0.05; **P < 0.01; ***P < 0.001 vs. Control group; #P < 0.05; ##P < 0.01; ###P < 0.001 vs. DNCB group; DNCB, dinitrochlorobenzene; SOD, superoxide dismutase; GPX4, Glutathione Peroxidase 4; GSH, glutathione.
Figure 3. Anti skin inflammation effect of three Taxus chinensis extracts (N ≥ 3)
(A) Representative ears photos of mice in each group after 30 minutes of inflammation induction; (B) Ear swelling rate of mice in each group after 30 minutes of inflammation induction; (C-G) Swelling rate of mice toes at different time points post inflammation induction; Data represent the mean ± SE; *P < 0.05; **P < 0.01; ***P < 0.001 vs. Control group; #P < 0.05 vs. Taxus chinensis essential oil group.
Figure 4. Anti skin allergy effect of three Taxus chinensis extracts (N = 5-7)
(A)Representative skin photos of mice in each group after 4-AP injected to induce allergy; (B) Pathological changes of skin tissue were observed by HE staining in each group (bar = 20 μm); (C) Body licking times of mice in each group within 10 minutes after allergic stimulation; (D) Histamine content in the skin tissue homogenates of mice in each group; (E) (F) mRNA level of SOD and GPX4 in the skin tissue of each group were tested; Data represent the mean ± SE; *P < 0.05; **P < 0.01; ***P < 0.001 vs. Control group; #P < 0.05; ##P < 0.01; ###P < 0.001 vs. 4-AP group; 4-AP, 4-aminopyridine; DNCB, dinitrochlorobenzene; HE, hematoxylin and eosin; SOD, superoxide dismutase; GPX4, Glutathione Peroxidase 4; TNF, tumor necrosis factor; IL, Interleukin.
-
[1] Sutterby E, Thurgood P, Baratchi S, et al. Microfluidic Skin-on-a-Chip Models: Toward Biomimetic Artificial Skin. Small, 2020; 16(39): e2002515. doi: 10.1002/smll.202002515 [2] Choi S Y, Kim Y C. Whitening effect of black tea water extract on brown Guinea pig skin. Toxicol Res, 2011; 27(3): 153-160. doi: 10.5487/TR.2011.27.3.153 [3] Rachmin I, Ostrowski S M, Weng Q Y, et al. Topical treatment strategies to manipulate human skin pigmentation. Adv Drug Deliv Rev, 2020; 153: 65-71. doi: 10.1016/j.addr.2020.02.002 [4] Lee R, Ko H J, Kim K, et al. Anti-melanogenic effects of extracellular vesicles derived from plant leaves and stems in mouse melanoma cells and human healthy skin. J Extracell Vesicles, 2020; 9(1): 1703480. doi: 10.1080/20013078.2019.1703480 [5] Kurban R S, Bhawan J. Histologic changes in skin associated with aging. J Dermatol Surg Oncol, 1990; 16(10): 908-914. doi: 10.1111/j.1524-4725.1990.tb01554.x [6] WULF H C, SANDBY-Møller J, KOBAYASI T, et al. Skin aging and natural photoprotection. Micron, 2004; 35(3): 185-191. doi: 10.1016/j.micron.2003.11.005 [7] Pillaiyar T, Manickam M, Jung S H. Downregulation of melanogenesis: drug discovery and therapeutic options. Drug Discov Today, 2017; 22(2): 282-298. doi: 10.1016/j.drudis.2016.09.016 [8] Kammeyer A, Luiten R M. Oxidation events and skin aging. Ageing Res Rev, 2015; 21: 16-29. doi: 10.1016/j.arr.2015.01.001 [9] Zhang P, Li T, Wu X, et al. Oxidative stress and diabetes: antioxidative strategies. Front Med, 2020; 14(5): 583-600. doi: 10.1007/s11684-019-0729-1 [10] Lee S M, Lee S H, Jung Y, et al. FABP3-mediated membrane lipid saturation alters fluidity and induces ER stress in skeletal muscle with aging. Nat Commun, 2020; 11(1): 5661. doi: 10.1038/s41467-020-19501-6 [11] Folgueras A R, Freitas-Rodriguez S, Velasco G, et al. Mouse models to disentangle the hallmarks of human aging. Circ Res, 2018; 123(7): 905-924. doi: 10.1161/CIRCRESAHA.118.312204 [12] Celebi Sozener Z, Cevhertas L, Nadeau K, et al. Environmental factors in epithelial barrier dysfunction. J Allergy Clin Immunol, 2020; 145(6): 1517-1528. doi: 10.1016/j.jaci.2020.04.024 [13] Zhou Y, Qin S, Sun M, et al. Measurement of organ-specific and acute-phase blood protein levels in early lyme disease. J Proteome Res, 2020; 19(1): 346-359. doi: 10.1021/acs.jproteome.9b00569 [14] Gu Y, Han J, Jiang C, et al. Biomarkers, oxidative stress and autophagy in skin aging. Ageing Res Rev, 2020; 59: 101036. doi: 10.1016/j.arr.2020.101036 [15] Brunner P M, Guttman-Yassky E, Leung D Y. The immunology of atopic dermatitis and its reversibility with broad-spectrum and targeted therapies. J Allergy Clin Immunol, 2017; 139(4S): S65-S76. [16] Bai X Y, Liu P, Chai Y W, et al. Artesunate attenuates 2, 4-dinitrochlorobenzene-induced atopic dermatitis by down-regulating Th17 cell responses in BALB/c mice. Eur J Pharmacol, 2020; 874: 173020. doi: 10.1016/j.ejphar.2020.173020 [17] Leung D Y M, Berdyshev E, Goleva E. Cutaneous barrier dysfunction in allergic diseases. J Allergy Clin Immunol, 2020; 145(6): 1485-1497. doi: 10.1016/j.jaci.2020.02.021 [18] Weng H B, Han W K, Xiong Y W, et al. Taxus chinensis ameliorates diabetic nephropathy through down-regulating TGF-β 1/Smad pathway. Chin J Nat Med, 2018; 16(2): 90-96. [19] Liu H S, Gao Y H, Liu L H, et al. Inhibitory effect of 13 taxane diterpenoids from Chinese yew (Taxus chinensis var. mairei) on the proliferation of HeLa cervical cancer cells. Biosci Biotechnol Biochem, 2016; 80(10): 1883-1886. doi: 10.1080/09168451.2016.1194182 [20] Aoki Y, Tanigawa T, Abe H, et al. Melanogenesis inhibition by an oolong tea extract in b16 mouse melanoma cells and UV-induced skin pigmentation in brownish guinea pigs. Biosci Biotechnol Biochem, 2007; 71(8): 1879-1885. doi: 10.1271/bbb.70099 [21] Shi C, Yao Z, Xu J, et al. Effects of Gingko Extract (EGb761) on oxidative damage under different conditions of serum supply. J Bioenerg Biomembr, 2009; 41(1): 61-69. doi: 10.1007/s10863-009-9197-7 [22] Cao J, Wang Y, Hu S, et al. Kaempferol ameliorates secretagogue-induced pseudo-allergic reactions via inhibiting intracellular calcium fluctuation. J Pharm Pharmacol, 2020; 72(9): 1221-1231. doi: 10.1111/jphp.13312 [23] Ding X J, Zhang Z Y, Jin J, et al. Salidroside can target both P4HB-mediated inflammation and melanogenesis of the skin. Theranostics, 2020; 10(24): 11110-11126. doi: 10.7150/thno.47413 [24] Elansary H O, Szopa A, Kubica P, et al. Phenolic compounds of catalpa speciosa, taxus cuspidate, and magnolia acuminata have antioxidant and anticancer activity. Molecules, 2019; 24(3): 412. doi: 10.3390/molecules24030412 [25] Li N, Pan Z, Zhang D, et al. Chemical components, biological activities, and toxicological evaluation of the fruit (aril) of two precious plant species from genus taxus. Chem Biodivers, 2017; 14(12)10.1002/cbdv. 201700305. [26] Weng H B, Han W K, Xiong Y W, et al. Taxus chinensis ameliorates diabetic nephropathy through down-regulating TGF-β1/Smad pathway. Chin J Natura Med, 2018; 16(2): 90-96. doi: 10.1016/S1875-5364(18)30034-7 [27] Hearing V J. Biochemical control of melanogenesis and melanosomal organization. J Investig Dermatol Symp Proc, 1999; 4(1): 24-28. doi: 10.1038/sj.jidsp.5640176 [28] Hearing V J, JimÉNez M. Analysis of mammalian pigmentation at the molecular level. Pigment Cell Res, 1989; 2(2): 75-85. doi: 10.1111/j.1600-0749.1989.tb00166.x [29] Shimogaki H, Tanaka Y, Tamai H, et al. In vitro and in vivo evaluation of ellagic acid on melanogenesis inhibition. Int J Cosmet Sci, 2000; 22(4): 291-303. doi: 10.1046/j.1467-2494.2000.00023.x [30] Cabanes J, Chazarra S, Garcia-Carmona F. Kojic acid, a cosmetic skin whitening agent, is a slow-binding inhibitor of catecholase activity of tyrosinase. J Pharm Pharmacol, 1994; 46(12): 982-985. [31] Zou Y, Wang A, Shi M, et al. Analysis of redox landscapes and dynamics in living cells and in vivo using genetically encoded fluorescent sensors. Nat Protoc, 2018; 13(10): 2362-2386. doi: 10.1038/s41596-018-0042-5 [32] Lennicke C, Cochemé H M. Redox metabolism: ROS as specific molecular regulators of cell signaling and function. Mol Cell, 2021; 81(18): 3691-3707. doi: 10.1016/j.molcel.2021.08.018 [33] Kimura Y, Shibuya N, Kimura H. Sulfite protects neurons from oxidative stress. Br J Pharmacol, 2019; 176(4): 571-582. doi: 10.1111/bph.14373 [34] Pooladanda V, Thatikonda S, Bale S, et al. Nimbolide protects against endotoxin-induced acute respiratory distress syndrome by inhibiting TNF-alpha mediated NF-kappaB and HDAC-3 nuclear translocation. Cell Death Dis, 2019; 10(2): 81. doi: 10.1038/s41419-018-1247-9 [35] Li H, Horke S, Förstermann U. Oxidative stress in vascular disease and its pharmacological prevention. Trends Pharmacol Sci, 2013; 34(6): 313-319. doi: 10.1016/j.tips.2013.03.007 [36] Gui T, Luo L, Chhay B, et al. Superoxide dismutase-loaded porous polymersomes as highly efficient antioxidant nanoparticles targeting synovium for osteoarthritis therapy. Biomaterials, 2022; 283: 121437. doi: 10.1016/j.biomaterials.2022.121437 [37] He X Y, Wang M, Liang L W. Study on anti-inflammatory effect of Taxus cuspidate. Anhui Agricul Sci, 2010; 38(02): 908-909. [38] Redegeld F A, Yu Y, Kumari S, et al. Non-IgE mediated mast cell activation. Immunol Rev, 2018; 282(1): 87-113. [39] Church M K, Kolkhir P, Metz M, et al. The role and relevance of mast cells in urticaria. Immunol Rev, 2018; 282(1): 232-247. -


 投稿系统
投稿系统


 下载:
下载: