Corona virus disease 2019-associated liver injury in cold regions
doi: 10.2478/fzm-2022-0026
-
Abstract: The corona virus disease 2019 (COVID-19) pandemic has created a global health and economic crisis. Our studies uncovered that in addition to respiratory symptoms, liver damage is also common in COVID-19 patients; however, the cause of liver damage has not been fully elucidated. In this article, we summarize the clinical manifestations and pathological features of COVID-19 reported in published relevant studies and delineate the etiology and pathogenesis of COVID-19-related liver injury. We speculate that cold stimulation may be associated with COVID-19-related liver injury, which should be considered in clinical decisionmaking and treatment of COVID-19 in cold regions.
-
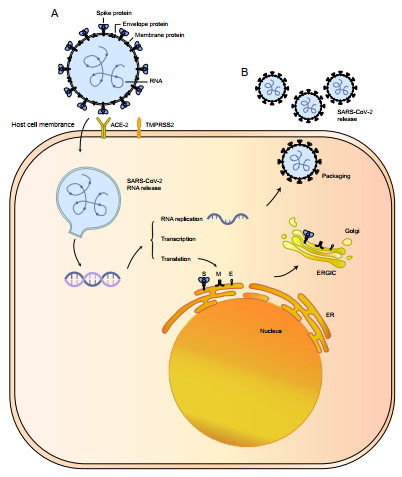
Figure 1. Predicted structural model of SARS-CoV-2 and its life cycle in host cells
(A) Possible structural model of SARS-CoV-2; (B) The life cycle of SARS-CoV-2 in host cells: the S protein of SARS-CoV-2 forms a complex with the ACE2 receptor on the host cell membrane, with the help of proteases, the viral complex is then transported into the host cell, and the viral RNA is subsequently released into the cytoplasm. Spike (S), envelope (E), and membrane (M) proteins are translated in the ER of host cells. Viral RNA and S, M, and E proteins assemble in the ERGIC to generate a new SARS-CoV-2, which is then released from the host cell by exocytosis. ER, endoplasmic reticulum; ACE2, angiotensin-converting enzyme 2; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; TMPRSS2, transmembrane protease serine 2; ERGIC, endoplasmic reticulum-Golgi intermediate compartment.
-
[1] Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet, 2020; 395(10223): 497-506. doi: 10.1016/S0140-6736(20)30183-5 [2] Medicine JHU. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). 2022. https://coronavirus.jhu.edu/map.html. Accessed on May 20, 2022. [3] Wu F, Zhao S, Yu B, et al. A new coronavirus associated with human respiratory disease in China. Nature, 2020; 579(7798): 265-269. doi: 10.1038/s41586-020-2008-3 [4] Zhou P, Yang X L, Wang X G, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 2020; 579(7798): 270-273. doi: 10.1038/s41586-020-2012-7 [5] Zhu N, Zhang D, Wang W, et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med, 2020; 382(8): 727-733. doi: 10.1056/NEJMoa2001017 [6] Wu J, Li W, Shi X, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Intern Med, 2020; 288(1): 128-138. doi: 10.1111/joim.13063 [7] World meter. COVID-19 CORONAVIRUS PANDEMIC. https://www.worldometers.info/coronavirus/. Accessed on May 23, 2022. [8] Icard P, Simula L, Rei J, et al. On the footsteps of Hippocrates, Sanctorius and Harvey to better understand the influence of cold on the occurrence of COVID-19 in European countries in 2020. Biochimie, 2021; 191: 164-171. doi: 10.1016/j.biochi.2021.09.009 [9] Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet, 2020; 395(10224): 565-574. doi: 10.1016/S0140-6736(20)30251-8 [10] Lan J, Ge J, Yu J, et al. Structure of the SARS-CoV-2 spike receptorbinding domain bound to the ACE2 receptor. Nature, 2020; 581(7807): 215-220. doi: 10.1038/s41586-020-2180-5 [11] Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell, 2020; 181(2): 271-280. e8. doi: 10.1016/j.cell.2020.02.052 [12] Walls A C, Park Y J, Tortorici M A, et al. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell, 2020; 181(2): 281-292. e6. doi: 10.1016/j.cell.2020.02.058 [13] Xie M, Chen Q. Insight into 2019 novel coronavirus - An updated interim review and lessons from SARS-CoV and MERS-CoV. Int J Infect Dis, 2020; 94: 119-124. doi: 10.1016/j.ijid.2020.03.071 [14] Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet, 2020; 395(10223): 507-513. doi: 10.1016/S0140-6736(20)30211-7 [15] Guan W J, Ni Z Y, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med, 2020; 382(18): 1708-1720. doi: 10.1056/NEJMoa2002032 [16] Wu J, Liu J, Zhao X, et al. Clinical Characteristics of Imported Cases of Coronavirus Disease 2019 (COVID-19) in Jiangsu Province: A Multicenter Descriptive Study. Clin Infect Dis, 2020; 71(15): 706-712. doi: 10.1093/cid/ciaa199 [17] Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. Br J Dermatol, 2020; 182(6): 1477-1478.198 FRIGID ZONE MEDICINE doi: 10.1111/bjd.19011 [18] Wu Z Y, McGoogan J M. Characteristics ofand Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA, 2020; 323(13): 1239-1242. doi: 10.1001/jama.2020.2648 [19] Marjot T, Webb G J, Barritt A St, et al. COVID-19 and liver disease: mechanistic and clinical perspectives. Nat Rev Gastroenterol Hepatol, 2021; 18(5): 348-364. doi: 10.1038/s41575-021-00426-4 [20] Wu J, Song S, Cao H C, et al. Liver diseases in COVID-19: Etiology, treatment and prognosis. World J Gastroenterol, 2020; 26(19): 2286-2293. doi: 10.3748/wjg.v26.i19.2286 [21] Kulkarni A V, Kumar P, Tevethia H V, et al. Systematic review with meta-analysis: liver manifestations and outcomes in COVID-19. Aliment Pharmacol Ther, 2020; 52(4): 584-599. doi: 10.1111/apt.15916 [22] Xu L, Liu J, Lu M, et al. Liver injury during highly pathogenic human coronavirus infections. Liver Int, 2020; 40(5): 998-1004. doi: 10.1111/liv.14435 [23] Jothimani D, Venugopal R, Abedin M F, et al. COVID-19 and the liver. J Hepatol, 2020; 73(5): 1231-1240. doi: 10.1016/j.jhep.2020.06.006 [24] Cai Q, Huang D, Yu H, et al. COVID-19: Abnormal liver function tests. J Hepatol, 2020; 73(3): 566-574. doi: 10.1016/j.jhep.2020.04.006 [25] Ding Z Y, Li G X, Chen L, et al. Association of liver abnormalities with in-hospital mortality in patients with COVID-19. J Hepatol, 2021; 74(6): 1295-1302. doi: 10.1016/j.jhep.2020.12.012 [26] Weber S, Hellmuth J C, Scherer C, et al. Liver function test abnormalities at hospital admission are associated with severe course of SARS-CoV-2 infection: a prospective cohort study. Gut, 2021; 70(10): 1925-1932. doi: 10.1136/gutjnl-2020-323800 [27] Yip T C, Lui G C, Wong V W, et al. Liver injury is independently associated with adverse clinical outcomes in patients with COVID-19. Gut, 2021; 70(4): 733-742. doi: 10.1136/gutjnl-2020-321726 [28] Mao R, Qiu Y, He J S, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol, 2020; 5(7): 667-678. doi: 10.1016/S2468-1253(20)30126-6 [29] Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ, 2020; 368: m1091. [30] Ponziani F R, Del Zompo F, Nesci A, et al. Liver involvement is not associated with mortality: results from a large cohort of SARS-CoV-2-positive patients. Aliment Pharmacol Ther, 2020; 52(6): 1060-1068. [31] Zhang Y, Zheng L, Liu L, et al. Liver impairment in COVID-19 patients: A retrospective analysis of 115 cases from a single centre in Wuhan city, China. Liver Int, 2020; 40(9): 2095-2103. doi: 10.1111/liv.14455 [32] Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a singlecentered, retrospective, observational study. Lancet Respir Med, 2020; 8(5): 475-481. doi: 10.1016/S2213-2600(20)30079-5 [33] Xu X W, Wu X X, Jiang X G, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ, 2020; 368: m606. [34] Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis, 2020; 20(4): 425-434. doi: 10.1016/S1473-3099(20)30086-4 [35] Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA, 2020; 323(11): 1061-1069. doi: 10.1001/jama.2020.1585 [36] Yang H Y, Jin B, Mao Y L. Liver injury in COVID-19: What do we know now? Hepatobiliary Pancreat Dis Int, 2020; 19(5): 407-408. doi: 10.1016/j.hbpd.2020.07.009 [37] Lei F, Liu Y M, Zhou F, et al. Longitudinal association between markers of liver injury and mortality in covid-19 in china. Hepatology, 2020; 72(2): 389-398. doi: 10.1002/hep.31301 [38] Richardson S, Hirsch J S, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA, 2020; 323(20): 2052-2059. doi: 10.1001/jama.2020.6775 [39] Ding Y, He L, Zhang Q, et al. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J Pathol, 2004; 203(2): 622-630. doi: 10.1002/path.1560 [40] Sonzogni A, Previtali G, Seghezzi M, et al. Liver histopathology in severe COVID 19 respiratory failure is suggestive of vascular alterations. Liver Int, 2020; 40(9): 2110-2116. doi: 10.1111/liv.14601 [41] Wang Y, Liu S, Liu H, et al. SARS-CoV-2 infection of the liver directly contributes to hepatic impairment in patients with COVID-19. J Hepatol, 2020; 73(4): 807-816. doi: 10.1016/j.jhep.2020.05.002 [42] Zhao Y, Zhao Z, Wang Y, et al. Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2. Am J Respir Crit Care Med, 2020; 202(5): 756-759. doi: 10.1164/rccm.202001-0179LE [43] Hikmet F, Mear L, Edvinsson A, et al. The protein expression profile of ACE2 in human tissues. Mol Syst Biol, 2020; 16(7): e9610. [44] Hamming I, Timens W, Bulthuis ML, et al. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol, 2004; 203(2): 631-637. doi: 10.1002/path.1570 [45] Chai X, Hu L, Zhang Y, et al. Specific ACE2 Expression in Cholangiocytes May Cause Liver Damage After 2019-nCoV Infection. bioRxiv, 2020. doi: 10.1101/2020.02.03.931766. [46] Zhao B, Ni C, Gao R, et al. Recapitulation of SARS-CoV-2 infection and cholangiocyte damage with human liver ductal organoids. Protein Cell, 2020; 11(10): 771-775. doi: 10.1007/s13238-020-00718-6 [47] Zhang J J, Dong X, Cao Y Y, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy, 2020; 75(7): 1730-1741. doi: 10.1111/all.14238 [48] Zhou MWY. A precision medicine approach to managing Wuhan Coronavirus. Precis Clin Med, 2020; 4(3): 14-21. [49] Song Y, Liu P, Shi X L, et al. SARS-CoV-2 induced diarrhoea as onset symptom in patient with COVID-19. Gut, 2020; 69(6): 1143-1144. doi: 10.1136/gutjnl-2020-320891 [50] Ma C, Cong Y, Zhang H. COVID-19 and the digestive system. Am J Gastroenterol, 2020; 115(7): 1003-1006. doi: 10.14309/ajg.0000000000000691 [51] Zhang H, Li H B, Lyu J R, et al. Specific ACE2 expression in small intestinal enterocytes may cause gastrointestinal symptoms and injury after 2019-nCoV infection. Int J Infect Dis, 2020; 96: 19-24. doi: 10.1016/j.ijid.2020.04.027 [52] Nardo A D, Schneeweiss-Gleixner M, Bakail M, et al. Pathophysiological mechanisms of liver injury in COVID-19. Liver Int, 2021; 41(1): 20-32. doi: 10.1111/liv.14730 [53] William M. Lee MD. Drug-Induced Hepatotoxicity. N Engl J Med, 1995; 333: 17. [54] Qiu H, Tong Z, Ma P, et al. Intensive care during the coronavirus epidemic. Intensive Care Med, 2020; 46(4): 576-578. doi: 10.1007/s00134-020-05966-y [55] Fan Z, Chen L, Li J, et al. Clinical features of COVID-19-related liver functional abnormality. Clin Gastroenterol Hepatol, 2020; 18(7): 1561-1566. doi: 10.1016/j.cgh.2020.04.002 [56] Lizardo-Thiebaud M J, Cervantes-Alvarez E, Limon-de la Rosa N, et al. Direct or collateral liver damage in SARS-CoV-2-infected patients. Semin Liver Dis, 2020; 40(3): 321-330. doi: 10.1055/s-0040-1715108 [57] Varga Z, Flammer A J, Steiger P, et al. Endothelial cell infection and199 FRIGID ZONE MEDICINE endotheliitis in COVID-19. Lancet, 2020; 395(10234): 1417-1418. doi: 10.1016/S0140-6736(20)30937-5 [58] Ackermann M, Verleden S E, Kuehnel M, et al. Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med, 2020; 383(2): 120-128. doi: 10.1056/NEJMoa2015432 [59] Gu S X, Tyagi T, Jain K, et al. Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. Nat Rev Cardiol, 2021; 18(3): 194-209. doi: 10.1038/s41569-020-00469-1 [60] Sepanlou S G, Safiri S, Bisignano C, et al. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol, 2020; 5(3): 245-266. doi: 10.1016/S2468-1253(19)30349-8 [61] Ji D, Qin E, Xu J, et al. Non-alcoholic fatty liver diseases in patients with COVID-19: A retrospective study. J Hepatol, 2020; 73(2): 451-453. doi: 10.1016/j.jhep.2020.03.044 [62] Lipsitch M, Viboud C. Influenza seasonality: lifting the fog. Proc Natl Acad Sci U S A, 2009; 106(10): 3645-3646. doi: 10.1073/pnas.0900933106 [63] Wolkoff P. Indoor air humidity, air quality, and health - An overview. Int J Hyg Environ Health, 2018; 221(3): 376-390. doi: 10.1016/j.ijheh.2018.01.015 [64] Tan J, Mu L, Huang J, et al. An initial investigation of the association between the SARS outbreak and weather: with the view of the environmental temperature and its variation. J Epidemiol Community Health, 2005; 59(3): 186-192. doi: 10.1136/jech.2004.020180 [65] Araújo MB, Naimi B. Spread of SARS-CoV-2 Coronavirus likely constrained by climate. medRxiv, 2020. doi: 10.1101/2020.03.12.20034728. [66] Wang M, Jiang A, Gong L, et al. Temperature Significantly Change COVID-19 Transmission in 429 cities. medRxiv, 2020. ChemRxiv. doi: 10.1101/2020.02.22.20025791 [67] Näyhä S, Hassi J. Cold and mortality from ischaemic heart disease in northern Finland. Arctic Med Res, 1995; 54 Suppl 2: 19-25. [68] Näyhä S. Cold and the risk of cardiovascular diseases. A review. Int J Circumpolar Health, 2002; 61(4): 373-380. doi: 10.3402/ijch.v61i4.17495 [69] Sun Z. Cardiovascular responses to cold exposure. Front Biosci (Elite Ed), 2010; 2(2): 495-503. [70] Waseem N, Chen PH. Hypoxic Hepatitis: A Review and Clinical Update. J Clin Transl Hepatol, 2016; 4(3): 263-268. [71] Lightsey J M, Rockey D C. Current concepts in ischemic hepatitis. Curr Opin Gastroenterol, 2017; 33(3): 158-163. doi: 10.1097/MOG.0000000000000355 [72] Dunn G D, Hayes P, Breen K J, et al. The liver in congestive heart failure a review. Am J Med Sci, 1973; 265(3): 174-189. doi: 10.1097/00000441-197303000-00001 -


 投稿系统
投稿系统


 下载:
下载: