Effects of intermittent cold-exposure on culprit plaque morphology in ST-segment elevation myocardial infarction patients: a retrospective study based on optical coherence tomography
doi: 10.2478/fzm-2022-0011
-
Abstract:
Objective Present study aimed to explore the effects of intermittent cold-exposure (ICE) on culprit plaque morphology in patients with STsegment elevation myocardial infarction (STEMI) in frigid zone. Methods Totally 848 STEMI patients with plaque rupture (N = 637) or plaque erosion (N = 211) were enrolled consecutively according to optical coherence tomography imaging. Data on the changes of outdoor air temperature corresponding to 24 solar terms were collected. Patients were divided into different groups according to 24 solar terms and the number of days with indoor central heating. Imaging data were measured and analyzed qualitatively and quantitatively. Statistical analysis was conducted to elucidate the possible association of the STEMI patients of different groups with plaque morphology of culprit vessel with alterations of ambient temperature. Results The incidence of both plaque rupture and plaque erosion presented trough in summer. The incidence of plaque rupture reached a peak value in early winter when outdoor air temperature dropped below 0℃ and declined with supply of central heating. Persistent cold exposure in early winter was positively and significantly associated with plaque rupture. The incidence of plaque erosion presented a peak in severe winter with outdoor air temperature dropping below -20℃ and steady supply of central heating. ICE in severe winter was positively and significantly associated with plaque with intact intima, especially in aged male or current smoking patients. The positive correlation of cold exposure with lipid size in culprit plaque in winter weakened with central heating. Conclusion ICE resulted from switching staying in between outdoor cold environment and indoor warm temperature with central heating in severe winter changed culprit plaque morphology in STEMI. Plaque rupture decreased whereas plaque erosion increased impacted by ICE. The effect of ICE on the transformation of plaque morphology might be explained by reduced lipid deposition. -
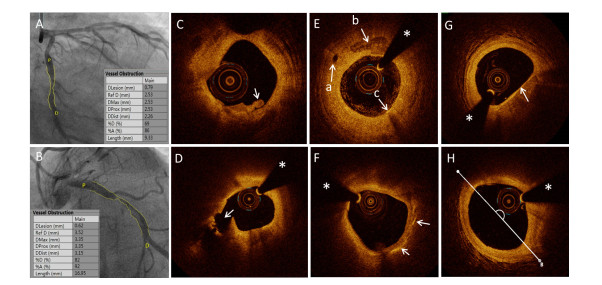
Figure 1. Typical images of patients
(A) A typical CAG image of a patient with STEMI and PE; (B) A typical image of a patient with STEMI and PR; (C) A typical OCT image of a patient with STEMI and PE characterized by intact and rough intima attached by small white thrombus. (D) A typical OCT image of a patient with STEMI and PR characterized by ruptured intima (arrow) backed with a big cavity (pound sign). (E) Representative OCT images, including micro-channel (left arrow), macrophage accumulation (arrow below), and spotty calcification (arrow above); (F) Representative OCT images of cholesterol crystal; (G) Representative OCT images of TCFA; (H) Lipid core determined based on the lipid arc. The asterisk marks the position of the OCT guide wire. CAG, coronary angiography; STEMI, ST-segment elevated myocardial infarction; PE, plaque erosion; OCT, optical coherence tomography; PR, plaque rupture; TCFA, thin-cap fibroatheroma;
Figure 3. Logistic regression of air temperature (AT) variables between PR and PE groups
(A) Logistic regression analysis of the association between AT variables and PR risk; (B) Logistic regression analysis of the association between AT variables and PR risk in subgroups. Abbreviations: AT, air temperature; ATAFP, AT around freezing point; ATBFP, AT below freezing point; ATLS, ATAFP in early spring; ATLA, ATAFP in early winter; ATSW, AT below −20℃ in severe winter; CI, confidence interval; CS, current smoker; DM, diabetes mellitus; HTN, hypertension; NCS, not current smoker; NDM, not diabetes mellitus; NHTN, not hypertension; OR, odds ratio; ST, solar terms. Adjust model Ⅰ adjusted for: age, male gender, current smoker, diabetes mellitus, and hypertension history. Adjust model Ⅱ adjusted for: age, male gender, current smoker, hypertension history, LDL-C level, and admission random plasma glucose level. Adjust model Ⅲ adjusted for: age, male gender, current smoker, hypertension history, LDL-C level, admission random plasma glucose level, culprit vessel and multivessel lesion.
Figure 4. ROC curves to evaluate the predictive ability of risk factors and some models
(A) ROC curves for single traditional risk factor respectively, (B) ROC curves for single air AT variables respectively, (C) ROC curves for ATSW combined with different traditional risk factors. Model ATSW, combined ATSW with traditional risk factors including age, male gender, current smoker, hypertension history, LDL-C level, admission random plasma glucose level, culprit vessel and multivessel lesion. (D) ROC curves for ATLA combined with different traditional risk factors, respectively, to evaluate their predictive value for plaque rupture. Model ATLA, combined ATLA and the traditional risk factors model ATSW applied. Abbreviations: AT, air temperature; ATAFP, AT around freezing point; ATLA, AT around freezing point in late autumn; ATSW, AT below −20℃ in severe winter; CH, center heating.
Figure 5. A heat-map of correlation between AT-related variables and OCT morphologic characteristics of culprit vessel
Expression levels for each row are color-coded according to the legend shown on the right of the map. Abbreviation: PR, plaque rupture; LL, length of culprit lesion; MLA, minimal lumen area; PRA, proximal referential lumen area; DRA, distal referential lumen area, LCL, length of lipid core; ALA, average arc of lipid core; LLA, maximal arc of lipid core; FCT, minimal thickness of fibrotic cap; OCT, optical coherence tomography; TL, length of residual thrombus; TCFA: thin fibrous cap atheroma; CholC, cholesterol crystal; MicC, micro-channel; ThL, thrombus length; ThT, thrombus type; AT, air temperature; ATBFP, AT below freezing point; ATSW, AT below −20℃ in severe winter; In-summer, AT above 28℃ in intense summer; ATAFP, AT around freezing point; ATLS, ATAFP in late spring; ATLA, ATAFP in late autumn.
Table 1. Weather variables between plaque rupture and plaque erosion
Risk weather ST period Plaque rupture
(N = 637)Plaque erosion
(N = 211)P-value Summer 7–12 150 (23.5%) 43 (20.4%) 0.341 Intense summer 10–12 71 (11.1%) 19(9%) 0.381 ATBFP 18-5 330 (51.8%) 119 (56.4%) 0.247 Winter 10–24 157 (24.6%) 62 (29.4%) 0.173 ATSW 22–24 69 (10.8%) 36 (17.1%) 0.017 ATAFP 4–6 and 17–19 190(29.8%) 40(19.0) 0.002 ATLA 17–19 115(18.1%) 22 (10.4%) 0.009 ATLS 4–6 75 (11.8%) 18 (8.5%) 0.191 Data are presented as N (%). Abbreviation: ATAFP, air temperature around freezing point; ATBFP, air temperature below freezing point; ATLA, air temperature around freezing point in late autumn; ATLS, air temperature arround freezing point in late spring; ATSW, air temperature in severe winter; ST, solar term. -
[1] Jia H, Abtahian F, Aguirre A D, et al. In vivo diagnosis of plaque erosion and calcified nodule in patients with acute coronary syndrome by intravascular optical coherence tomography. J Am Coll Cardiol, 2013; 62(19): 1748-1758. doi: 10.1016/j.jacc.2013.05.071 [2] Dai J, Xing L, Jia H, et al. In vivo predictors of plaque erosion in patients with st-segment elevation myocardial infarction: A clinical, angiographical, and intravascular optical coherence tomography study. Eur Heart J, 2018; 39(22): 2077-2085. doi: 10.1093/eurheartj/ehy101 [3] Virmani R, Kolodgie F D, Burke A P, et al. Lessons from sudden coronary death: A comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler, Thromb, and Vasc biol, 2000; 20(5): 1262-1275. doi: 10.1161/01.ATV.20.5.1262 [4] Jia H, Dai J, Hou J, et al. Effective anti-thrombotic therapy without stenting: Intravascular optical coherence tomography-based management in plaque erosion (the erosion study). Eur Heart J, 2017; 38(11): 792-800. [5] Niccoli G, Montone R A, Di Vito L, et al. Plaque rupture and intact fibrous cap assessed by optical coherence tomography portend different outcomes in patients with acute coronary syndrome. Eur Heart J, 2015; 36(22): 1377-1384. doi: 10.1093/eurheartj/ehv029 [6] Yabushita H, Bouma B E, Houser S L, et al. Characterization of human atherosclerosis by optical coherence tomography. Circulation, 2002; 106(13): 1640-1645. doi: 10.1161/01.CIR.0000029927.92825.F6 [7] Spencer F A, Goldberg R J, Becker R C, et al. Seasonal distribution of acute myocardial infarction in the second national registry of myocardial infarction. J Am Coll Cardiol, 1998; 31(6): 1226-1233. doi: 10.1016/S0735-1097(98)00098-9 [8] Sun Z, Chen C, Xu D, et al. Effects of ambient temperature on myocardial infarction: A systematic review and meta-analysis. Environ Pollut, 2018; 241: 1106-1114. doi: 10.1016/j.envpol.2018.06.045 [9] Sheth T, Nair C, Muller J, et al. Increased winter mortality from acute myocardial infarction and stroke: The effect of age. J Am Coll Cardiol, 1999; 33(7): 1916-1919 doi: 10.1016/S0735-1097(99)00137-0 [10] Rumana N, Kita Y, Turin T C, et al. Seasonal pattern of incidence and case fatality of acute myocardial infarction in a japanese population (from the takashima ami registry, 1988 to 2003). Am J Cardiol, 2008; 102(10): 1307-1311. doi: 10.1016/j.amjcard.2008.07.005 [11] Vasconcelos J, Freire E, Almendra R, et al. The impact of winter cold weather on acute myocardial infarctions in portugal. Environ Pollut, 2013; 183: 14-18. doi: 10.1016/j.envpol.2013.01.037 [12] Ogbebor O, Odugbemi B, Maheswaran R, et al. Seasonal variation in mortality secondary to acute myocardial infarction in England and Wales: A secondary data analysis. BMJ Open, 2018; 8(7): e019242. doi: 10.1136/bmjopen-2017-019242 [13] Davie G S, Baker M G, Hales S, et al. Trends and determinants of excess winter mortality in new zealand: 1980 to 2000. BMC Public Health, 2007; 7: 263. doi: 10.1186/1471-2458-7-263 [14] Shibuya J, Kobayashi N, Asai K, et al. Comparison of coronary culprit lesion morphology determined by optical coherence tomography and relation to outcomes in patients diagnosed with acute coronary syndrome during winter -vs- other seasons. Am J Cardiol, 2019; 124(1): 31-38. doi: 10.1016/j.amjcard.2019.03.045 [15] Prati F, Regar E, Mintz G S, et al. Expert review document on methodology, terminology, and clinical applications of optical coherence tomography: Physical principles, methodology of image acquisition, and clinical application for assessment of coronary arteries and atherosclerosis. Eur Heart J, 2010; 31(4): 401-415. doi: 10.1093/eurheartj/ehp433 [16] Liu X, Sun C, Gu X, et al. Intraplaque neovascularization attenuated statin benefit on atherosclerotic plaque in cad patients: A follow-up study with combined imaging modalities. Atherosclerosis, 2019; 287: 134-139. doi: 10.1016/j.atherosclerosis.2019.06.912 [17] Sher L. Effects of seasonal mood changes on seasonal variations in coronary heart disease: Role of immune system, infection, and inflammation. Med Hypotheses, 2001; 56(1): 104-106. doi: 10.1054/mehy.2000.1122 [18] Keatinge W R, Coleshaw S R, Cotter F, et al. Increases in platelet and red cell counts, blood viscosity, and arterial pressure during mild surface cooling: Factors in mortality from coronary and cerebral thrombosis in winter. Br Med J, 1984; 289(6456): 1405-1408. doi: 10.1136/bmj.289.6456.1405 [19] Chen X, Shang W, Huang X, et al. The effect of winter temperature on patients with ischemic stroke. Med Sci Monit, 2019; 25: 3839-3845. doi: 10.12659/MSM.916472 [20] Mattila K J, Valtonen V V, Nieminen M S, et al. Role of infection as a risk factor for atherosclerosis, myocardial infarction, and stroke. Clin Infect Dis, 1998; 26(3): 719-734. doi: 10.1086/514570 [21] Sun Z, Cade R, Morales C. Role of central angiotensin ii receptors in cold-induced hypertension. Am J Cardiol. 2002; 15(1 Pt 1): 85-92. [22] Barnett A G, Sans S, Salomaa V, et al. The effect of temperature on systolic blood pressure. Blood Press Monit, 2007; 12(3): 195-203. doi: 10.1097/MBP.0b013e3280b083f4 [23] Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of europe. The eurowinter group. Lancet, 1997; 349(9062): 1341-1346. doi: 10.1016/S0140-6736(96)12338-2 [24] Donaldson G C, Ermakov S P, Komarov Y M, et al. Cold related mortalities and protection against cold in yakutsk, eastern siberia: Observation and interview study. BMJ. 1998; 317(7164): 978-982. doi: 10.1136/bmj.317.7164.978 [25] Liu J, Wang S, Hou J, et al. Proteomics profiling reveals insulinlike growth factor 1, collagen type vi alpha-2 chain, and fermitin family homolog 3 as potential biomarkers of plaque erosion in st-segment elevated myocardial infarction. Cir J, 2020; 84(6): 985-993. doi: 10.1253/circj.CJ-19-1206 [26] Virmani R, Burke A P, Kolodgie F D, et al. Vulnerable plaque: The pathology of unstable coronary lesions. J Inter Card, 2002; 15(6): 439- 446. doi: 10.1111/j.1540-8183.2002.tb01087.x [27] Virmani R, Burke A P, Farb A, et al. Pathology of the vulnerable plaque. J Am Coll Cardiol, 2006; 47(Suppl 8): C13-18. [28] Tulenko T N, Sumner A E. The physiology of lipoproteins. Journal of Nuclear Cardiology, 2002; 9(6): 638-649. doi: 10.1067/mnc.2002.128959 [29] Williams K J, Tabas I. The response-to-retention hypothesis of early atherogenesis. Arterioscler Thromb Vasc Biol, 1995; 15(5): 551-561. doi: 10.1161/01.ATV.15.5.551 [30] McKie G L, Shamshoum H, Hunt K L, et al. Intermittent cold exposure improves glucose homeostasis despite exacerbating dietinduced obesity in mice housed at thermoneutrality. J Physiol, 2021; 600(4): 829-845. [31] Amano H, Noike R, Yabe T, et al. Frailty and coronary plaque characteristics on optical coherence tomography. Heart Vessels, 2020; 35(6): 750-761. doi: 10.1007/s00380-019-01547-2 -


 投稿系统
投稿系统


 下载:
下载: