Ticagrelor versus clopidogrel in East Asian patients with acute coronary syndrome: A meta-analysis
doi: 10.2478/fzm-2022-0004
-
Abstract:
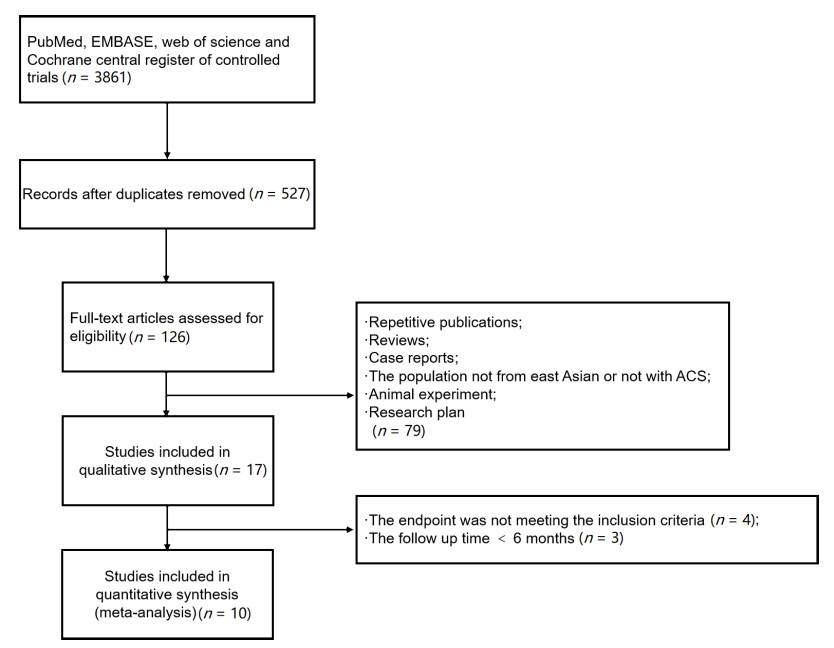
Objective There exist conflicting data on the efficacy and safety of ticagrelor and clopidogrel in East Asian patients with acute coronary syndrome (ACS). We performed a meta-analysis to evaluate whether ticagrelor or clopidogrel produces better outcomes for East Asian patients with ACS. Methods We searched for randomized controlled trials reporting associations between ticagrelor and clopidogrel in East Asian patients with acute coronary syndrome in PubMed, EMBASE, web of science and Cochrane central register of controlled trials. Results Ten studies involving 3 715 participants were qualified for our analysis. The major adverse cardiovascular events (MACE) were significantly decreased in patients with ticagrelor treatment compared to those with clopidogrel (risk ratio [RR]: 0.61; 95% confidence interval [CI]: 0.38-0.98; P = 0.042). There was no significant difference in all-cause death (RR: 0.89; 95% CI: 0.61-1.29; P = 0.540), cardiovascular death (RR: 0.86; 95% CI: 0.58-1.27; P = 0.451), myocardial infarction (RR: 0.91; 95% CI: 0.65-1.27; P = 0.575) and stroke (RR: 0.77; 95% CI: 0.44-1.36; P = 0.372) between ticagrelor and clopidogrel. Ticagrelor was associated with a significantly higher risk of bleeding compared to clopidogrel (RR: 1.71; 95% CI: 1.37-2.13; P = 0.000). Conclusion The present meta-analysis demonstrates that ticagrelor reduced the incidence of MACE in ACS patients from East Asia compared with clopidogrel. However, it increased the risk of bleeding. -
Key words:
- ticagrelor /
- clopidogrel /
- acute coronary syndrome /
- Eastern Asia /
- meta-analysis
-
Table 1. Baseline characteristics of included studies
References Country Follow-up(months) Sample size(n) Age(years) Male(n) Hypertension(%) Diabetes(%) Ticagrelor Clopidogrel Ticagrelor Clopidogrel Ticagrelor Clopidogrel Ticagrelor Clopidogrel Ticagrelor Clopidogrel Goto S et al., 2015[7] China, South Korea and Japan 12 401 400 67±12 66±11 306 307 76.1 72.5 38.4 31.0 Kang HJ et al., 2015[9] China and South Korea 12 278 273 NA NA NA NA NA NA NA NA Xia JG et al., 2015[19] China 6 48 48 53.7±10.3 54.6±9.8 36 38 62.5 64.6 50 45.8 Wang HD et al., 2016[11] China 12 100 100 NA NA 69 66 79 82 42 39 Tang XY et al., 2016[20] China 6 200 200 64.36±11.41 64.18±11.09 142 146 61 58 29 21 Ren Q et al., 2016[21] China 12 149 151 56±9.2 55±8.0 102 106 NA NA NA NA Lu YJ et al., 2016[22] China 12 95 108 59.25±9.63 59.63±9.88 52 60 34.7 38.9 25.3 29.6 Wu HB et al., 2018[12] China 12 124 120 58.976±10.187 61.058±11.600 98 94 51.6 57.5 25.8 20.8 Yang B et al., 2018[13] China 6 60 60 59.6±15.7 58.7±13.5 35 38 NA NA NA NA Park DW et al., 2019[23] South Korea 12 400 400 62.5±11.3 62.3±11.5 297 302 55.8 48.2 29.0 25.0 -
[1] Cuisset T, Verheugt F W A, Mauri L. Update on antithrombotic therapy after percutaneous coronary revascularization. Lancet, 2017; 390(10096): 810-820. doi: 10.1016/S0140-6736(17)31936-0 [2] Gandhi S, Zile B, Tan M K, et al. Increased uptake of guideline-recommended oral antiplatelet therapy: insights from the Canadian acute coronary syndrome reflective. Can J Cardiol, 2014; 30(12): 1725-1731. doi: 10.1016/j.cjca.2014.09.011 [3] Karve A M, Seth M, Sharma M, et al. Contemporary use of ticagrelor in interventional practice (from blue cross blue shield of michigan cardiovascular consortium). Am J Cardiol, 2015; 115(11): 1502-1506. doi: 10.1016/j.amjcard.2015.02.049 [4] Levine G N, Bates E R, Blankenship J C, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: An update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction. J Am Coll Cardiol, 2016; 67(10): 1235-1250. doi: 10.1016/j.jacc.2015.10.005 [5] Authors/Task Force members, Windecker S, Kolh P, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: The task force on myocardial revascularization of the European Society Of Cardiology (ESC) and the European association for cardio-thoracic surgery (EACTS) Developed with the special contribution of the European association of percutaneous cardiovascular interventions (EAPCI). Eur Heart J, 2014; 35(37): 2541-2619. [6] 2012 Writing Committee Members, Jneid H, Anderson J L, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American college of cardiology foundation/american heart association task force on practice guidelines. Circulation, 2012; 126(7): 875-910. doi: 10.1161/CIR.0b013e318256f1e0 [7] Wallentin L, Becker R C, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med, 2009; 361(11): 1045-1057. doi: 10.1056/NEJMoa0904327 [8] Goto S, Huang C H, Park S J, et al. Ticagrelor vs. Clopidogrel in Japanese, Korean and Taiwanese patients with acute coronary syndrome-randomized, double-blind, phase Ⅲ PHILO Study. Circ J, 2015; 79(11): 2452-2460. doi: 10.1253/circj.CJ-15-0112 [9] Wu B, Lin H, Tobe R G, et al. Ticagrelor versus clopidogrel in East-Asian patients with acute coronary syndromes: a meta-analysis of randomized trials. J Comp Eff Res, 2018; 7(3): 281-291. doi: 10.2217/cer-2017-0074 [10] Kang H J, Clare R M, Gao R, et al. Ticagrelor versus clopidogrel in Asian patients with acute coronary syndrome: a retrospective analysis from the platelet inhibition and patient outcomes (PLATO) Trial. Am Heart J, 2015; 169(6): 899-905. doi: 10.1016/j.ahj.2015.03.015 [11] Misumida N, Aoi S, Kim S M, et al. Ticagrelor versus clopidogrel in East Asian patients with acute coronary syndrome: Systematic review and meta-analysis. Cardiovasc Revasc Med, 2018; 19(6): 689-694. doi: 10.1016/j.carrev.2018.01.009 [12] Wang H, Wang X. Efficacy and safety outcomes of ticagrelor compared with clopidogrel in elderly Chinese patients with acute coronary syndrome. Ther Clin Risk Manag, 2016; 12: 1101-1105. doi: 10.2147/TCRM.S108965 [13] Wu H B, Tian H P, Wang X C, et al. Clinical efficacy of ticagrelor in patients undergoing emergency intervention for acute myocardial infarction and its impact on platelet aggregation rate. Am J Transl Res, 2018; 10(7): 2175-2183. http://www.ncbi.nlm.nih.gov/pubmed/30093954 [14] Yang B, Zheng C, Yu H, et al. Comparison of ticagrelor and clopidogrel for patients undergoing emergency percutaneous coronary intervention. Iran J Public Health, 2018; 47(7): 952-957. http://ijph.tums.ac.ir/index.php/ijph/article/download/14036/6035 [15] Gao C Z, Ma Q Q, Wu J, et al. Comparison of the effects of ticagrelor and clopidogrel on inflammatory factors, vascular endothelium functions and shortterm prognosis in patients with acute stsegment elevation myocardial infarction undergoing emergency percutaneous coronary intervention: a pilot study. Cell Physiol Biochem, 2018; 48(1): 385-396. doi: 10.1159/000491768 [16] Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ, 2015; 350: g7647. http://europepmc.org/abstract/med/25797233 [17] Higgins J P, Altman D G, Gøtzsche P C, et al. The cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ, 2011; 343: d5928. doi: 10.1136/bmj.d5928 [18] Huedo-Medina T B, Sánchez-Meca J, Marín-Martínez F, et al. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods, 2006; 11(2): 193-206. doi: 10.1037/1082-989X.11.2.193 [19] Higgins J P, Thompson S G, Deeks J J, et al. Measuring inconsistency in meta-analyses. BMJ, 2003; 327(7414): 557-560. doi: 10.1136/bmj.327.7414.557 [20] Xia J G, Qu Y, Hu S D, et al. Midterm follow-up outcomes of ticagrelor on acute ST segment elevation myocardial infarction undergoing emergency percutaneous coronary intervention. Beijing Da Xue Xue Bao. Yi Xue Ban, 2015; 47(3): 494-498. http://www.ncbi.nlm.nih.gov/pubmed/26080882 [21] Tang X, Li R, Jing Q, et al. Assessment of ticagrelor versus clopidogrel treatment in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. J Cardiovasc Pharmacol, 2016; 68(2): 115-120. doi: 10.1097/FJC.0000000000000390 [22] Ren Q, Ren C, Liu X, et al. Ticagrelor vs. clopidogrel in non-ST-elevation acute coronary syndromes. Herz, 2016; 41(3): 246-249. doi: 10.1007/s00059-015-4359-3 [23] Lu Y, Li Y, Yao R, et al. Clinical effect of ticagrelor administered in acute coronary syndrome patients following percutaneous coronary intervention. Exp Ther Med, 2016; 11(6): 2177-2184. doi: 10.3892/etm.2016.3224 [24] Park D W, Kwon O, Jang J S, et al. Clinically significant bleeding with ticagrelor versus clopidogrel in Korean patients with acute coronary syndromes intended for invasive management: a randomized clinical trial. Circulation, 2019; 140(23): 1865-1877. doi: 10.1161/CIRCULATIONAHA.119.041766 [25] Cannon C P, Harrington R A, James S, et al. Comparison of ticagrelor with clopidogrel in patients with a planned invasive strategy for acute coronary syndromes (PLATO): a randomized double-blind study. The lancet, 2010; 375(9711): 283-293. doi: 10.1016/S0140-6736(09)62191-7 [26] Blin P, Dureau-Pournin C, Benichou J, et al. Secondary prevention of acute coronary events with antiplatelet agents (SPACE-AA): One-year real-world effectiveness and safety cohort study in the French nationwide claims database. Atherosclerosis, 2018; 281(7): 98-106. http://www.sciencedirect.com/science/article/pii/S0021915018315120 [27] Harding S A, Holley A, Wilkins B, et al. Contemporary antiplatelet therapy in acute coronary syndromes: are there differences in outcomes and discontinuation between clopidogrel and ticagrelor? Intern Med J, 2017; 47(11): 1298-1305. doi: 10.1111/imj.13595 [28] Small D S, Payne C D, Kothare P, et al. Pharmacodynamics and pharmacokinetics of single doses of prasugrel 30 mg and clopidogrel 300 mg in healthy Chinese and white volunteers: an open-label trial. Clin Ther, 2010; 32(2): 365-379. doi: 10.1016/j.clinthera.2010.02.015 [29] Teng R, Butler K. Pharmacokinetics, pharmacodynamics, and tolerability of single and multiple doses of ticagrelor in Japanese and Caucasian volunteers. Int j Clin Pharmacol Ther, 2014; 52(6): 478-491. doi: 10.5414/CP202017 [30] Li H, Butler K, Yang L, et al. Pharmacokinetics and tolerability of single and multiple doses of ticagrelor in healthy Chinese subjects: An open-label, sequential, two-cohort, single-centre study. Clin Drug Invest, 2012; 32(2): 87-97. doi: 10.2165/11595930-000000000-00000 [31] He M J, Liu B, Sun D H, et al. One-quarter standard-dose ticagrelor better than standard-dose clopidogrel in Chinese patients with stable coronary artery disease: A randomized, single-blind, crossover clinical study. Int J Cardiol, 2016; 215: 209-213. doi: 10.1016/j.ijcard.2016.04.087 [32] He M, Li D, Zhang Y, et al. Effects of different doses of ticagrelor on platelet aggregation and endothelial function in diabetic patients with stable coronary artery disease. Platelets, 2019; 30(6): 752-761. doi: 10.1080/09537104.2018.1513479 [33] He M, Zhang Y, Yan W, et al. 60 mg dose ticagrelor provides stronger platelet inhibition than clopidogrel in Chinese patients with chronic coronary syndrome: A randomized, single-blind, crossover study. Thromb Res, 2020; 190: 60-61. doi: 10.1016/j.thromres.2020.03.014 [34] Shi J, He M, Wang W, et al. Efficacy and safety of different ticagrelor regimens versus clopidogrel in patients with coronary artery disease: a retrospective multicenter study (SUPERIOR). Platelets, 2020; 23: 1-10. doi: 10.1080/09537104.2020.1732328 [35] Bonaca M P, Bhatt D L, Cohen M, et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med, 2015; 372(19): 1791-1800. doi: 10.1056/NEJMoa1500857 -


 投稿系统
投稿系统


 下载:
下载: