Characteristics of gut microbiota in anastomotic leakage patients in cold zones post-colorectal cancer surgery: A high-throughput sequencing and propensity-score matching study
doi: 10.1515/fzm-2024-0013
-
Abstract:
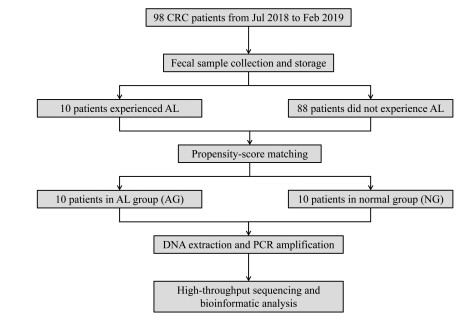
Objective The study aimed to explore the association between gut microbiota and anastomotic leakage (AL) after surgery in colorectal cancer (CRC) patients from a frigid zone, based on high-throughput sequencing. Methods A total of 98 CRC patients admitted to the Second Affiliated Hospital of Harbin Medical University from July 2018 to February 2019, who met the inclusion criteria, were included. Among these, 10 patients were diagnosed as AL. After propensity-score matching of baseline characteristics, 10 patients from the anastomotic leakage group (AG) and 10 patients from the normal group (NG) were finally included in this study. Fecal samples were collected, and total DNA was extracted for high-throughput sequencing and bioinformatic analysis. Results Alpha diversity analysis showed no significant difference between the two groups, while beta diversity analysis revealed significant differences in principal components. Differential microbiota were classified as Proteobacteria at the phylum level (P = 0.021). At the genus level, the abundances of Streptococcus (P = 0.045), Citrobacter (P = 0.008) and Klebsiella (P = 0.002) were significantly different between the two groups. LEfSe analysis indicated that these genera contributed most to the differences between the groups. Conclusion The characteristics of the gut microbiota in the AG and NG were significantly different, and these differences might be associated with AL in CRC patients from frigid zones. -
Key words:
- colorectal cancer /
- anastomotic leakage /
- gut microbiota
-
Table 1. Basic demographic characteristics before and after propensity score matching (PSM)
Characteristics Before PSM P value After PSM P value AG (N = 10) NG (N = 88) AG (N = 10) NG (N = 10) Gender, N (%) 0.973 0.606 Male 8 (80.0) 70 (79.5) 8 (80.0) 7 (70.0) Female 2 (20.0) 18 (20.5) 2 (20.0) 3 (30.0) Age, years, N (%) 0.193 0.653 ≥ 60 4 (40.0) 54 (61.4) 4 (40.0) 5 (50.0) < 60 6 (60.0) 34 (38.6) 6 (60.0) 5 (50.0) BMI (kg/m2), X ± s 22.7 ± 2.6 21.9 ± 3.0 0.506 22.7 ± 2.6 22.9 ± 3.1 0.844 Tumor location, N (%) 0.990 0.865 Right-sided colon 2 (20.0) 18 (20.5) 2 (20.0) 2 (20.0) Left-sided colon 3 (30.0) 28 (31.8) 3 (30.0) 2 (20.0) Rectum 5 (50.0) 42 (47.7) 5 (50.0) 6 (60.0) ASA score, N (%) 0.517 0.264 Ⅰ-Ⅱ 9 (90.0) 72 (81.8) 9 (90.0) 7 (70.0) Ⅲ-Ⅳ 1 (10.0) 16 (18.2) 1 (10.0) 3 (30.0) TNM stage, N (%) 0.583 0.654 Ⅰ 0 10 (11.4) 0 0 Ⅱ 3 (30.0) 28 (31.8) 3 (30.0) 4 (40.0) Ⅲ 6 (60.0) 37 (42.0) 6 (60.0) 4 (40.0) Ⅳ 1 (10.0) 13 (14.8) 1 (10.0) 2 (20.0) AG, anastomotic leakage group; NG, normal group; ASA, American Society of Anesthesiologists Table 2. Comparison of pathological outcomes after propensity score matching
Characteristics AG (N = 10) NG (N = 10) P value T stage, N (%) 0.329 T1/T2 2 (20.0) 4 (40.0) T3/T4 8 (80.0) 6 (60.0) N stage, N (%) 0.639 N0 3 (30.0) 4 (40.0) N1/N2 7 (70.0) 6 (60.0) Tumor maximum diameter (cm), N (%) 0.264 < 5 1 (10.0) 3 (30.0) ≥ 5 9 (90.0) 7 (70.0) Grade, N (%) 0.717 Well differentiated 1 (10.0) 2 (20.0) Moderately differentiated 7 (70.0) 7 (70.0) Poor differentiated 2 (20.0) 1 (10.0) Histology, N (%) 0.136 Adenocarcinoma 8 (80.0) 10 (100.0) Other types 2 (20.0) 0 Table 3. Alpha diversity analysis outcomes
Index name AG NG P value Simpson 0.10 ± 0.06 0.20 ± 0.16 0.089 Shannon 3.12 ± 0.61 2.58 ± 0.72 0.086 Sobs 175.70 ± 49.18 153.40 ± 42.77 0.294 Chao 193.33 ± 45.68 174.85 ± 41.48 0.356 Ace 196.06 ± 34.75 183.95 ± 44.42 0.506 AG, anastomotic leakage group; NG, normal group -
[1] Sung H, Ferlay J, Siegel R L, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin, 2021; 71(3): 209-249. doi: 10.3322/caac.21660 [2] Zheng R, Zhang S, Zeng H, et al. Cancer incidence and mortality in China, 2016. J Nat Cancer Cent, 2022; 2(1): 1-9. doi: 10.1016/j.jncc.2022.02.002 [3] Bertelsen C A, Andreasen A H, Jørgensen T, et al. Anastomotic leakage after anterior resection for rectal cancer: risk factors. Colorectal Dis, 2010; 12(1): 37-43. doi: 10.1111/j.1463-1318.2008.01711.x [4] Law W L, Choi H K, Lee YM, et al. Anastomotic leakage is associated with poor long-term outcome in patients after curative colorectal resection for malignancy. J Gastrointest Surg, 2007; 11(1): 8-15. doi: 10.1007/s11605-006-0049-z [5] Gaines S, Shao C, Hyman N, et al. Gut microbiome influences on anastomotic leak and recurrence rates following colorectal cancer surgery. Br J Surg, 2018; 105(2): e131-e141. doi: 10.1002/bjs.10760 [6] Sciuto A, Merola G, De Palma G D, et al. Predictive factors for anastomotic leakage after laparoscopic colorectal surgery. World J Gastroenterol, 2018; 24(21): 2247-2260. doi: 10.3748/wjg.v24.i21.2247 [7] Nikolian V C, Kamdar N S, Regenbogen S E, et al. Anastomotic leak after colorectal resection: a population-based study of risk factors and hospital variation. Surgery, 2017; 161(6): 1619-1627. doi: 10.1016/j.surg.2016.12.033 [8] Parthasarathy M, Greensmith M, Bowers D, et al. Risk factors for anastomotic leakage after colorectal resection: a retrospective analysis of 17518 patients. Colorectal Dis, 2017; 19(3): 288-298. doi: 10.1111/codi.13476 [9] Shakhsheer B A, Versten L A, Luo J N, et al. Morphine promotes colonization of anastomotic tissues with collagenase - producing enterococcus faecalis and causes leak. J Gastrointest Surg, 2016; 20(10): 1744-1751. doi: 10.1007/s11605-016-3237-5 [10] van Praagh J B, de Goffau M C, Bakker I S, et al. Intestinal microbiota and anastomotic leakage of stapled colorectal anastomoses: a pilot study. Surg Endosc, 2016; 30(6): 2259-2265. doi: 10.1007/s00464-015-4508-z [11] Zhang Y K, Zhang Q, Wang Y L, et al. A comparison study of age and colorectal cancer-related gut bacteria. Front Cell Infect Microbiol, 2021; 11: 606490. doi: 10.3389/fcimb.2021.606490 [12] Xiong H, Wang J, Chang Z, et al. Gut microbiota display alternative profiles in patients with early-onset colorectal cancer. Front Cell Infect Microbiol, 2022; 12: 1036946. doi: 10.3389/fcimb.2022.1036946 [13] Chiarello MM, Fransvea P, Cariati M, et al. Anastomotic leakage in colorectal cancer surgery. Surg Oncol, 2022; 40: 101708. doi: 10.1016/j.suronc.2022.101708 [14] Gessler B, Eriksson O, Angenete E. Diagnosis, treatment, and consequences of anastomotic leakage in colorectal surgery. Int J Colorectal Dis, 2017; 32(4): 549-556. doi: 10.1007/s00384-016-2744-x [15] Young J, Badgery-Parker T, Dobbins T, et al. Comparison of ECOG/ WHO performance status and ASA score as a measure of functional status. J Pain Symptom Manage, 2015; 49(2): 258-264. doi: 10.1016/j.jpainsymman.2014.06.006 [16] Qi Z, Zhibo Z, Jing Z, et al. Prediction model of poorly differentiated colorectal cancer (CRC) based on gut bacteria. BMC Microbiol, 2022; 22(1): 312. doi: 10.1186/s12866-022-02712-w [17] Sarhadi V, Lahti L, Saberi F, et al. Gut microbiota and host gene mutations in colorectal cancer patients and controls of iranian and finnish origin. Anticancer Res, 2020; 40(3): 1325-1334. doi: 10.21873/anticanres.14074 [18] Alverdy J C, Schardey H M. Anastomotic leak: toward an understanding of its root causes. J Gastrointest Surg, 2021; 25(11): 2966-2975. doi: 10.1007/s11605-021-05048-4 [19] Hajjar R, Gonzalez E, Fragoso G, et al. Gut microbiota influence anastomotic healing in colorectal cancer surgery through modulation of mucosal proinflammatory cytokines. Gut, 2023; 72(6): 1143-1154. doi: 10.1136/gutjnl-2022-328389 -


 投稿系统
投稿系统


 下载:
下载: